摘要: 目的:提高对CD30阳性的弥漫大B细胞淋巴瘤(DLBCL)的认识。方法:回顾性分析2022年4月陕西省人民医院收治1例免疫组织化学染色CD30弥漫表达的DLBCL患者的临床资料,并进行文献复习。结果:患者为76岁男性,于外院行超声检查提示颈部3、4区淋巴结肿大,并行颈部淋巴结穿刺活检,结合其组织形态学特点及免疫组织化学染色等诊断为CD30阳性的弥漫大B细胞淋巴瘤。予BV联合CHP方案化疗2疗程,CHOP联合来那度胺方案化疗6疗程,患者肿大淋巴结较前明显缩小,疗效评估接近完全缓解。结论:CD30弥漫阳性的DLBCL较为罕见,其免疫表型及组织学形态与经典型ALCL相似,应尽早行组织病理学检查,明确诊断,尽早治疗。
Abstract:
Objective: To enhance understanding of CD30-positive Diffuse Large B-Cell Lymphoma (DLBCL). Methods: A retrospective analysis was conducted on the clinical data of a patient with immuno-histochemically stained CD30-positive DLBCL, treated in April 2022 at the Shaanxi Provincial Peo-ple’s Hospital. This included a review of relevant literature. Results: The patient, a 76-year-old male, presented with enlarged lymph nodes in regions 3 and 4 of the neck, as identified by ultrasound examination in another hospital. A neck lymph node biopsy, combined with histomorphological characteristics and immunohistochemical staining, led to the diagnosis of CD30-positive DLBCL. The patient underwent two cycles of chemotherapy with the BV + CHP regimen and six cycles with the CHOP + Lenalidomide regimen. There was a significant reduction in the size of the enlarged lymph nodes, and the therapeutic effect was assessed as nearing complete remission. Conclusion: CD30-positive DLBCL is relatively rare, with an immunophenotype and histological morphology similar to classical Anaplastic Large Cell Lymphoma (ALCL). Early histopathological examination for definitive diagnosis and prompt treatment is recommended.
1. 引言
弥漫大B细胞淋巴瘤(diffuse large B cell lymphoma, DLBCL)是发病率最高的非霍奇金淋巴瘤,具有高度的异质性。本文报道1例CD30弥漫强阳性表达的大B细胞淋巴瘤,避免误诊为经典型间变大细胞淋巴瘤。
2. 病例资料
患者男性,76岁。发现颈部淋巴结肿大20余天。2022年4月于外院行超声检查提示颈部3、4区淋巴结肿大,并于该院行颈部淋巴结穿刺活检。
病理检查:(大体)送检穿刺标本,灰白灰红色条索样组织4条,长1~1.5 cm,直径0.1 cm。镜下表现:肿瘤细胞呈弥漫片状排列,淋巴结正常结构被破坏,肿瘤细胞体积大而松散,黏附性差。肿瘤细胞胞浆少,染色质稍粗,核呈圆形或卵圆形,嗜酸性大核仁显著(图1),背景见小淋巴细胞(图2),可见多处坏死灶,偶见爆米花样(图3)、肾形大细胞(图4)。免疫组化结果:肿瘤细胞广谱细胞角蛋白(CKpan)、CD3、CD5、CD7、CD20、MPO、LCA、Cyclin-D1、BCL-6、CD138、ALK (D5F3)、OCT-2均阴性表达。PAX-5 (图5)、MUM-1、CD10、CD38、Bob-1为阳性表达,CD30呈弥漫强阳性表达(图6)、CD21见少许残存破损FDC网、Ki-67指数70%。原位杂交检测EB病毒编码RNA (EBER)阴性。IG/TCR基因重排结果:未检测到TCR基因重排,检测到免疫球蛋白基因重排。结合病理组织学特点及免疫组织化学表现诊断为CD30阳性的弥漫大B细胞淋巴瘤。患者2022年5月于外院采用BV联合CHP方案(维布妥昔单抗、环磷酰胺、盐酸表柔比星、醋酸泼尼松)化疗2疗程,后因经济原因改用CHOP联合来那度胺方案(环磷酰胺、盐酸表柔比星、长春新碱、醋酸泼尼松、来那度胺)化疗6疗程,肿大淋巴结较前明显缩小,疗效评估接近完全缓解,目前身体状况良好。
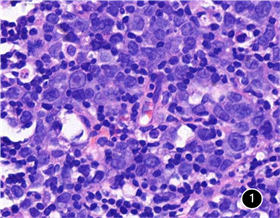
Figure 1. Tumor cells with prominent eosinophilic nucleoli within the nuclei, HE 400×
图1. 肿瘤细胞胞核内嗜酸性大核仁显著,HE 400×

Figure 2. Tumor cells intermingled with surrounding small lymphocytes, infiltrating growth, HE 200×
图2. 肿瘤细胞与周围小淋巴细胞穿插浸润生长,HE 200×
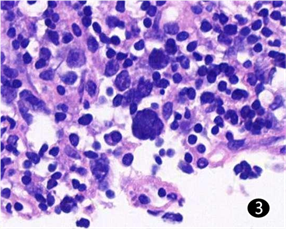
Figure 3. Presence of popcorn-like large cells, HE 400×
图3. 见爆米花样大细胞,HE 400×
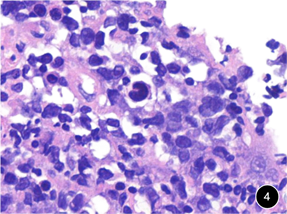
Figure 4. Presence of kidney-shaped nuclei observed, HE 400×
图4. 见肾形细胞核,HE 400×
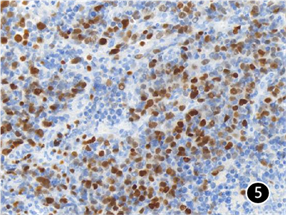
Figure 5. PAX-5 positive in large cells, EnVision method 200×
图5. PAX-5大细胞阳性,EnVision法200×
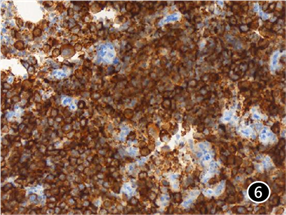
Figure 6. Diffuse positive expression of CD30, EnVision method 200×
图6. CD30弥漫阳性表达,EnVision法200×
3. 讨论
弥漫大B细胞淋巴瘤(diffuse large B cell lymphoma, DLBCL)是一类具有高度异质性的非霍奇金淋巴瘤,同时也是发病率最高的NHL亚型,在西方国家占NHL的30%~40%,中国的发病率约为50.7% [1] ,WHO根据其病理组织学特点将其分为4种变异型:中心母细胞型、免疫母细胞型、富于T细胞/组织细胞性及间变型 [2] 。
CD30生理状态下表达水平较低,在疾病状态下,如病毒感染、自身免疫性疾病及多种淋巴瘤中,CD30会呈现较高水平表达。CD30的表达对于几种淋巴瘤的确诊至关重要,在CHL和ALCL中近乎100%的肿瘤细胞表达CD30、因而CD30已被用作这两类淋巴瘤的诊断标志物 [3] 。CD30在各型B细胞淋巴瘤中表达情况差别较大,15%~20%的B细胞淋巴瘤表达CD30 [4] [5] ,其中在DLBCL中14%~25%的病例呈阳性表达 [6] [7] 。CD30在非特殊型DLBCL中阳性表达的比率报道不一。国际弥漫大B细胞淋巴瘤R-CHOP联盟项目研究组(IDCP)的研究显示,以阳性细胞 ≥ 20%为cut off值,CD30表达于14%的原发性DLBCL中 [8] ;拉丁美洲学者也以阳性细胞 ≥ 20%为cut off值,发现表达于21%的原发性DLBCL中 [9] ,而Hao对146例广州人群的原发性DLBCL研究中,CD30阳性表达率为15.7% [10] 。有文献报道,CD30阳性的DLBCL具有更好的临床转归及预后,Hu等人提出CD30阳性的DLBCL可能是一种独立亚型,CD30靶向药的使用或许能够改善患者的预后 [7] 。
EBV阳性的DLBCL,WHO已将其列为单独的临床亚型 [11] ,它常常伴有CD30表达 [12] ,但本例病例原位杂交检测EB病毒编码RNA(EBER)为阴性表达,与其有差异。贡其星的研究发现,在CD30阳性的DLBCL中,形态学分型以间变型相对多见,而免疫母细胞型相对少见 [13] 。间变型DLBCL,细胞中等偏大,呈圆形、椭圆形或多角形,部分可相似于霍奇金R-S细胞或间变大细胞淋巴瘤肿瘤细胞,可出现怪异型核,常伴有CD30的表达,与本例病例形态学相似。本例穿刺组织在小淋巴细胞背景内散在或成片的大细胞浸润,核仁明显,且本例免疫表型CD3及CD20均阴性表达,应当与可能会出现这种表达方式的淋巴瘤相鉴别。
大多数情况下,除了HL及ALCL之外,其他类型淋巴瘤表达CD30经常都是部分细胞阳性,并且强度为弱到中等,很少出现肿瘤细胞弥漫强阳性表达的情况,大片肿瘤细胞弥漫强阳性首先会想到ALCL,对于CD30弥漫强阳性表达,MUM-1阳性,而CD20阴性,LCA、OCT-2、CD138等均为阴性,很容易误诊为ALCL;本例就属于这种情况,其肿瘤细胞CD30弥漫强阳性表达,但T细胞相关标记均为阴性,且表达PAX-5、Bob-1等B细胞标记物;其ALK (D5F3)为阴性表达,结合基因重排结果,故本例最终诊断为弥漫大B细胞淋巴瘤。本例组织形态学及免疫组织化学染色特殊,应与相似表型淋巴造血疾病相鉴别:1) 经典型霍奇金淋巴瘤,HL的HRS大细胞常单个散在分布,很少弥漫成片,PAX5常弱阳性表达,CD10阴性表达,而本例肿瘤性大细胞弥漫成片,PAX5强阳性表达,与HL不符。2) ALK阴性的间变大细胞淋巴瘤,肿瘤细胞典型的生长方式为窦内生长或T细胞区黏附性生长,常表达一个或多个T细胞标记物。而本例肿瘤细胞弥漫片状排列,并无前者典型的生长方式,且PAX-5、Bob-1等B细胞标记物阳性表达,可与之鉴别。3) PAX-5阳性间变大细胞淋巴瘤,国内外共报道14例PAX-5阳性的ALCL,其中8例为ALK阴性ALCL,4例原发皮肤ALCL、2例ALK阳性ALCL [14] 。虽然其会表达PAX-5,但是不表达其他B细胞标记,并且TCR克隆性重排阳性,可以与本例鉴别。4) ALK阳性弥漫大B细胞淋巴瘤,肿瘤细胞呈免疫母细胞或浆母细胞样,空泡状细胞核,中央可见大核仁,ALK呈细胞质颗粒状阳性,CD30通常为阴性或局灶阳性。而本例ALK阴性,CD30弥漫强阳性表达,因此与ALK阳性DLBCL不符。5) 浆母细胞淋巴瘤,主要累及淋巴结以外部位,尤其是在黏膜组织。中等偏大的肿瘤样淋巴细胞弥漫浸润生长,肿瘤细胞呈圆形或椭圆形,呈免疫母细胞或浆母细胞样,CD38、CD138、MUM-1弥漫阳性表达,Ki-67指数接近100%,EBER阳性表达。而本例除可见嗜酸性大细胞外,爆米花样、肾形大细胞散在分布。EBER阴性,PAX-5、CD30阳性,Ki-67指数70%低于PBL,因此与PBL不符。
CD30可作为CD30阳性淋巴瘤的精准治疗靶标,目前它已被确定为DLBCL的重要治疗靶点 [15] ,如果将其与不同机制抗肿瘤方案相联合,或将改善患者预后。
综上所述,CD30弥漫强阳性的DLBCL罕见,在病理诊断过程中易与其他具有大细胞且CD30阳性的淋巴瘤混淆,应当仔细分析其组织病理学特点及行相关免疫组织化学检查,综合分析避免误诊、漏诊。
基金项目
陕西省重点研发项目(No. 2023-YBSF-668);陕西省人民医院领军人才支持计划项目(No. 2021LJ-12)。
NOTES
*通讯作者。