1. 引言
糖尿病视网膜病变(Diabetic Retinopathy, DR)是糖尿病的严重并发症之一,能导致视力损伤乃至不可逆性盲。糖尿病患者失明的发生率是一般人群的25倍。新近的研究表明,氧化应激和应激激活的信号通路与DR有着十分密切关系。氧自由基通过激活聚腺苷二磷酸核糖转移酶(PARP)[1] [2] 参与或者促发多元醇、蛋白激酶C﹑糖基化终末产物和氨基己糖等4条异常代谢通路[3] [4] 。Kowluru [5] 等发现无论是糖尿病个体的视网膜,还是高糖环境中培养的视网膜内皮细胞与周细胞均可观察到氧化应激增强。而这些异常途径又反过来激发氧自由基大量生成,形成恶性循环,加重视网膜损害。有研究发现血清甘油三脂与DR严重程度呈正相关,血清低密度脂蛋白异常与糖尿病黄斑水肿有关[6] 。提示在DR发生器质性改变前即使用抗氧化及降脂治疗可能有助于改善DR的代谢及功能,阻止DR的发展,保护视功能。丙丁酚是一种用于临床的强抗氧化剂,可以抑制脂质过氧化物的产生[7] ,FDA已经批准丙丁酚为特异性抑制LDL-C氧化修饰药物[8] 。故本研究对丙丁酚治疗DR早期(非增殖型)患者的临床疗效进行观察,现报告如下。
2. 资料与方法
2.1. 一般资料
2012年1月至2013年8月筛选确诊为非增殖型DR病变门诊病例68例,平均年龄为55.93 ± 8.18岁(范围是40~65岁)。随机分为4组,即:A组、强化治疗+丙丁酚组,共17例;B组、强化治疗 + 安慰剂组,共17例;C组、常规治疗 + 丙丁酚组,共17例;D组、常规治疗 + 安慰剂组,共17例,避免服用其它抗氧化剂。四组的性别(男/女)及NPDR组患者的最佳矫正视力进行卡方检验,证实各组间无显著差异(P > 0.05),对四组的平均年龄、平均随访时间进行单因素方差分析,证实四组无显著性差异(P > 0.05)。四组DR患者干预前的FBG、SBP、TC、LDL-C均无显著性差异(P > 0.05)。
2.2. 方法
所有的患者都进行详细的病史记录,包括姓名、年龄、性别、籍贯、民族、职业、工作条件、通讯方式及可靠程度,既往疾病史及诊治经过等,是否有其他眼部疾病或系统性疾病,以及家庭成员健康情况。
所有的患者在用药前及1年后进行视力、常规裂隙灯检查、眼压、血压、眼底镜检查、眼底彩色照相或眼底荧光血管造影检查、FPG、血脂(TC、LDLC)检查,A、C组DR患者在控制血糖、血压基础上予丙丁酚0.375 g,(商品名之乐,山东齐鲁制药有限公司。每片0.125 g,生产批号910042KL;国药准字:H10980054),每日2次。
2.3. 观察指标
观察四组干预前及最终随访时最佳矫正视力,眼底(眼底照相/眼底荧光造影),血脂(TC、LDLC)的变化。
2.4. 视网膜病变评估
患者用药前和用药后1年分别进行视力、眼底检查、眼底彩色照像、眼底荧光血管造影检查。1) 显效:视力进步 ≥ 4排,或视力 ≥ 1.0;眼底改变显示视网膜微血管瘤数由(+++)减少到(++)或由(++)减少到(+)、或由(+)到消失,眼底出血量由(+++)减少到(+)、或由(++)到消失;渗出量由(+++)减少到(++)或由(++)减少到(+)、或由(+)到消失。微血管瘤、出血、渗出改变有2项以上指标达到要求;眼底荧光血管造影显示视网膜平均循环时间明显缩短、黄斑水肿程度明显减轻、视网膜毛细血管无灌注区缩小、血管渗漏明显减轻。改变有2项以上指标达到要求,变化程度 ≥ 20%。2) 有效:视力进步 ≥ 2排;眼底改变显示视网膜微血管瘤数由(+++)减少到(++)、或由(++)减少到(+)、或由(+)到消失;眼底出血量由(+++)减少到(+)、或由(++)到消失;渗出量由(+++)到(++)、或由(++)减少到(+)、或由(+)到消失。微血管瘤、出血、渗出改变有1项以上指标达到要求;眼底荧光血管造影显示视网膜平均循环时间缩短、黄斑水肿程度减轻、视网膜毛细血管无灌注区缩小,血管渗漏明显减轻。改变有1项以上指标达到要求,变化成度 ≥ 10%。3) 无效:各项指标未达到上述有效标准者4) 恶化:视力退步2排以上;眼底彩色照相显示视网膜出现新生血管等增殖性改变;眼底荧光血管造影显示视网膜毛细血管无灌注区扩大,黄斑水肿加重,血管渗漏增加。
注:1) 视力检查采用国际标准视力表(1分制),不及0.1者,每进0.02计为1排;2) 眼底变化指标以眼底镜或彩色眼底照片判定,微血管瘤应以眼底荧光血管造影为准;3) (+)表示较少、易数;(++)表示较多、不易数;(+++)表示微血管瘤很多、不可数,出血及渗出量多、融合成片;4) 疗效评定时,视力、眼底改变及荧光造影3项中须具备2项。
2.5. 统计学处理
应用SPSS For Windows13.0软件包建立数据,计量资料组间比较用方差分析,同一组前后比较用配对样本均数的t检验,用均数±标准差表示;计数资料采用卡方检验,P < 0.05为差异有统计学意义。
3. 结果
3.1. 干预后四组NPDR患者眼底情况的比较
最终随访时,A、B、C、D四组最终随访时眼底情况(χ2 = 47.852, P < 0.01),四组间有显著性差异。总有效率A组为94.11%,C组为76.47%,而B、D组均为0。提示丙丁酚治疗后,患者眼底病变得以明显改善,(见表1、图1)。
3.2. 干预后四组NPDR患者最佳矫正视力的比较
最终随访时,四组患者最佳矫正视力有显著性差异(P < 0.05);进一步两两比较,发现A、B组最佳矫正视力有显著性差异(P < 0.05);A、D组最佳矫正视力有显著性差异(P < 0.05);A、C组最佳矫正视力无显著性差异(P > 0.05)。(见表2、表3)
3.3. 四组NPDR患者干预后的血脂的比较
最终随访时,A、C组TC、LDL-C水平均显著低于干预前(P < 0.05);B、D组干预前后血脂水平无显著性差异(P > 0.05);A组干预后TC、LDL-C水平显著低于B组(P < 0.05);C组干预后TC、LDL-C水平显著低于D组(P < 0.05);且干预后A、C组间TC、LDL-C水平无显著性差异(P > 0.05),提示丙丁酚能够有效降低NPDR的TC、LDL-C水平。

Table 1. Fundus comparison of four groups of NPDR patients (number of eyes)
表1. 四组NPDR患者眼底情况比较(眼数)
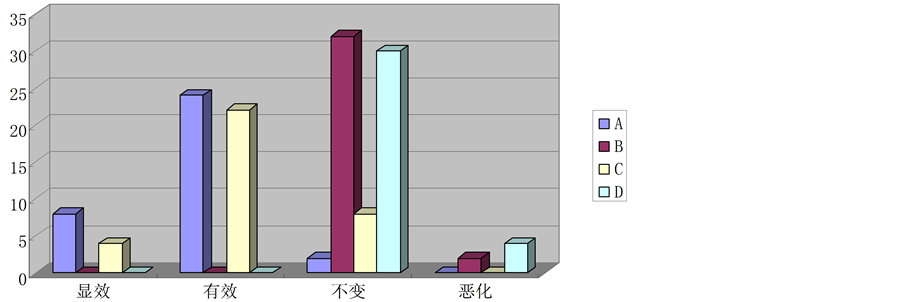
Figure 1. Fundus comparison of four groups of NPDR patients after therapy
图1. 四组NPDR患者干预后眼底情况比较

Table 2. Right eye’s best corrected visual acuity of four groups of NPDR patients before and after therapy
表2. 四组NPDR患者右眼干预前后最佳矫正视力分布情况

Table 3. Left eye’s best corrected visual acuity of four groups of NPDR patients before and after therapy
表3. 四组NPDR患者左眼干预前后最佳矫正视力分布情况
4. 讨论
糖尿病视网膜病变(Diabetic Retinopathy, DR)是糖尿病的严重并发症之一,能导致视力损伤乃至不可逆性盲。由于糖尿病发病率的逐年急剧增加及人类寿命的延长,DR已成为威胁人们身体健康的全球性公共卫生问题。越来越多的实验及临床研究提示氧化应激和应激激活的信号通路是糖尿病病程的贯穿主线。
视网膜富含多不饱和脂肪酸,具有最高的葡萄糖氧化过程,是氧摄取量最高的组织,因此,视网膜在氧化应激中最容易受损伤。有研究表明,对糖尿病大鼠的视网膜组织以及孵化于高糖基质的视网膜细胞的超氧化物进行检测,发现其水平显著增高[9] 。Kowaltowski [10] 等在糖尿病动物视网膜中发现,其毛细血管细胞凋亡、线粒体内膜存在漏隙及细胞色素C释放。使用抗氧化剂阻止线粒体内ROS的产生,即可阻断多元醇、蛋白激酶C(PKC)和晚期糖基化终末化产物(AGEs)通路的异常。对这个复杂的网络中线粒体超氧化作用和PARP异常激活等二个中心环节进行恰当的干预,可能是突破DR治疗瓶颈最有前景的方法之一[11] 。丙丁酚(Probucol),化学名:4,4’-[(1一甲基亚乙基)双(硫)]双[2,6一双(1,二甲基乙基)苯酚],于1969年开始应用于临床,最初作为降脂药,目前是FDA唯一认证的抗氧化药物。研究发现,丙丁酚具有很强的抗氧化作用[12] -[15] ,其分子结构中存在两个易被氧化的酚羟基,决定了其较强的捕捉氧离子的能力,从而形成稳定的酚氧基团。由于酚羟基具有脂溶性,且在脂蛋白颗粒中分布于脂蛋白表面,使其易于穿过内皮细胞达到血管壁发挥抗氧化作用,从而有效降低血清氧自由基浓度。因此,我们对糖尿病视网膜病变早期患者进行前瞻性研究,以观察治疗前后丙丁酚治疗组与对照组之间对糖尿病视网膜病变早期患者临床效果。
本研究结果表明,A、B、C、D四组眼底情况有显著性差异。总有效率A组为94.11%,C组为76.47%,而B、D组均为0。A、C组TC、LDL-C水平均显著低于干预前(P < 0.05);B、D组干预前后血脂水平无显著性差异(P > 0.05);上述结果说明,丙丁酚能够有效的改善NPDR患者眼底情况,可以调节NPDR患者的血脂情况,降低TC及LDL-C水平。丙丁酚不良反应较少,偶有腹泻、便秘、胃肠胀气、胃灼热、呃逆、头痛、眩晕、关节僵硬,但均少见且不严重,一般不需停药,如停药后即消失。对于没有禁忌证的NPDR合并血脂异常的患者提倡早期应用,并注意个体化用药及其可能带来的副作用。在抗氧化应激反应中丙丁酚起了重要的作用,还需深入其分子机制的研究及临床应用的推广。