摘要:
【目的】观察不同年龄段人群实测与6.0 mm瞳孔直径下全角膜和前角膜球面像差的差异。【方法】观察不同年龄段(20~29, 30~39, 40~49, 50~59, 60~69, 70~79)共100例受试者,通过Sirius眼前节分析系统检测不同瞳孔直径下(2.0 mm, 2.5 mm, 3.0 mm, 3.5 mm, 4.0 mm, 4.5 mm, 5.0 mm, 5.5 mm, 6.0 mm, 6.5 mm, 7.0 mm)全角膜和前角膜球面像差及暗环境下实测瞳孔直径,通过数学拟合曲线计算出该实测瞳孔直径下全角膜和前角膜的球面像差值,分别比较其与6.0 mm瞳孔直径下全角膜与前角膜球面像差之间的差异。【结果】实测瞳孔直径与年龄呈负相关(P < 0.05)。全角膜和前角膜实测球面像差与年龄均呈负相关(P < 0.05),6.0 mm瞳孔直径下前角膜球面像差与年龄呈正相关(P < 0.05),而全角膜球面像差则与年龄无关(P > 0.05)。在60~69,70~79年龄段,实测全角膜和前角膜球面像差均显著低于6.0 mm瞳孔直径下对应参数(P < 0.05)。在20~29,30~39,70~79年龄段,实测全角膜与前角膜球面像差间有显著性差异(P < 0.05);在6.0 mm瞳孔直径下,全角膜球面像差值在30~39,40~49,60~69年龄段显著低于前角膜对应值(P < 0.05)。【结论】老年人群中实测瞳孔直径下全和前角膜球面像差均显著小于6.0 mm瞳孔直径下对应参数,此差异与老年人群实际平均瞳孔直径较小有关。在实测和6.0 mm瞳孔直径下,全与前角膜球面像差在部分年龄段存在差异,两者有显著性差异的年龄段分布不同。所测前角膜球面像差不能完全代替全角膜球面像差,建议以实测全角膜球面像差值作为白内障手术选择消球差人工晶状体类型的依据。
Abstract:
Objective: To compare the difference between total and anterior corneal spherical aberrations calculated on the basis of the pupil diameters of 6.0 mm and the actual measurements in different age groups. Methods: A total of 100 subjects in different age groups (20 - 29 years old, 30 - 39 years old, 40 - 49 years old, 50 - 59 years old, 60 - 69 years old, 70 - 79 years old) were examined using Sirius anterior segment analytic system. Their total corneal spherical aberrations (TCSA) and anterior corneal spherical aberrations(ACSA) were detected on the basis of different machine-provided pupil diameters (2.0 mm, 2.5 mm, 3.0 mm, 3.5 mm, 4.0 mm, 4.5 mm, 5.0 mm, 5.5 mm, 6.0 mm, 6.5 mm, 7.0 mm) and the scotopic pupil diameters were recorded as measured pupil diameters in the dark room. TCSA and ACSA based on the machine-measured pupil diameter was calculated through fitting curves, and compared to the TCSA and ACSA at a theoretical 6-mm pupil diameter. Results: The measured pupil diameter was negatively correlated with age (P < 0.05). TCSA and ACSA based on measured pupil diameter were both negatively correlated with age (P < 0.05). At 6-mm pupil diameter, ACSA was positively correlated with age (P < 0.05), while there was no obvious correlation between TCSA and age. In 60 - 69 and 70 - 79 years old groups, their TCSA and ACSA at the measured pupil diameters were significantly lower than those at 6-mm pupil diameter (P < 0.05). In 20 - 29, 30 - 39 and 70 - 79 years old groups, TCSA were significantly different from ACSA at the measured pupil diameters (P < 0.05). In 30 - 39, 40 - 49 and 60 - 69 years old groups, TCSA were significantly lower than ACSA at 6-mm pupil diameter (P < 0.05). Conclusions: TCSA and ACSA at the measured pupil diameters in the old subjects are significantly lower than those at 6-mm pupil diameter, which could be ascribed to their relatively small actual mean pupil sizes. At either the measured pupil diameters or 6-mm pupil diameter, TCSA significantly different from ACSA in some age groups. Our study suggested that the TCSA, rather than ACSA, at measured pupil diameter should be used for the selection of aplanatic intraocular lens for cataract patients.
1. 引言
人眼并非理想的光学系统,由于角膜和晶状体的光学性能并非完美,因而不仅存在着离焦和散光等低阶像差,也存在着球差、慧差、三叶草差等高阶像差,造成视物眩光、模糊、夜视力下降、对比敏感度减弱等问题,限制着人眼的视觉质量 [1] [2]。高阶像差中的球面像差对视觉质量影响较大,但可以有针对性矫正,由于消球差非球面人工晶状体的应用,白内障术后全眼球面像差可以得到有效控制,但术前如何获得患眼准确的角膜球面像差值仍是临床密切关注的问题 [3] [4]。
目前临床常用的测量角膜球面像差的仪器,如i-Trace波前像差仪(Tracey Co. US),光程差分析仪(OPD Scan, Nidek Co. Japan),三维眼前节分析仪(Pentacam, OCULUS Ltd. Germany)等,均常规默认6.0 mm中央角膜区域直径下角膜球面像差为输出值 [5] [6] [7]。由于仪器测量原理的差异,部分仪器只能测量角膜前表面球面像差,并以其代表全角膜球面像差,而固定瞳孔直径下的前角膜与全角膜球面像差是否存在差异,前者是否可代替后者应用于临床却少有文献报道。此外,且由于个体差异,不同患者在暗环境下实际瞳孔直径并非固定为6.0 mm [8] [9],这也可能造成球面像差结果的偏倚。基于以上分析,本研究对不同年龄段实测和6.0 mm瞳孔直径下的全角膜和前角膜球面像差的差异进行了分析。
2. 对象和方法
1、对象:选取2019年3月31日至2019年5月31日于华中科技大学同济医学院附属协和医院就诊的受试者100例,共200只眼,按照年龄划分为6组:A组,20~29岁,共17例34眼;B组,30~39岁,共30例60眼;C组,40~49岁,共13例26眼;D组,50~59岁,共14例28眼;E组,60~69岁,共14例28眼;F组,70~79岁,共12例24眼。该研究采用回顾性研究,遵循“赫尔辛基宣言”,并获得华中科技大学同济医学院医学伦理委员会批准。入选标准为:1) 年龄20-80周岁;2) 停戴软性角膜接触镜2周以上,硬性角膜接触镜2月以上。排除标准为:1) 离焦 ≥ ±3.00 D,散光 ≥ ±1.50 D;2) 疑似圆锥角膜、圆锥角膜及其他角膜病变;3) 存在干眼、翼状胬肉、严重角膜血管翳等眼表病变;4) 既往眼部手术史及眼部外伤史;5) Sirius机测Kappa角 ≥ 0.5 mm。
2、方法:所有受试者用同一台Sirius眼前节分析仪(CSO, Florence, Italy)进行三维角膜地形图检测,由同一位经验丰富的技师操作。嘱病人坐于设备前,注视前方,睁大双眼,充分暴露角膜,瞬目睁眼后,待屏幕上下测量线均变为绿色,按下拍摄键。再嘱病人睁大双眼,充分暴露瞳孔,拍摄拟暗环境下的瞳孔大小(0.4 xl),收集数据。选取采集质量覆盖率 > 90%,可信度 = 100%的角膜地形图,记录不同瞳孔直径下(2.0 mm、2.5 mm、3.0 mm、3.5 mm、4.0 mm、4.5 mm、5.0 mm、5.5 mm、6.0 mm、6.5 mm、7.0 mm)的全角膜和前角膜球面像差值,重复3次取平均值。
使用MATLAB软件(R2017a, MathsWorks, America)通过上述11个瞳孔直径下全角膜和前角膜球面像差结果作出拟合曲线,并计算出该受试者在暗环境实测瞳孔直径下全角膜球面像差(以下简称“实测全球差”)和前角膜的球面像差值(以下简称“实测前球差”);以6.0 mm瞳孔直径下全角膜球面像差值(以下简称“理论全球差”)和前角膜球面像差值(以下简称“理论前球差”)作为理论值。对以上结果进行统计分析。
3、统计学分析:利用SPSS 20.0软件对获取数据进行处理和分析。计量资料采用
表示。全、前角膜的实测和理论球面像差间比较、各年龄段间比较采用配对样本t检验。相关性分析采用Pearson分析法,r < 0.1,极弱相关或无相关;0.1 ≤ r < 0.3,弱相关;0.3 ≤ r < 0.5,中等相关;r ≥ 0.5,强相关 [10]。P < 0.05视为有统计学意义。
3. 结果
1、年龄与瞳孔直径的关系
暗视环境下,瞳孔直径随年龄增长逐渐减小,二者呈强负相关(r = −0.6728,P < 0.001) (见图1)。
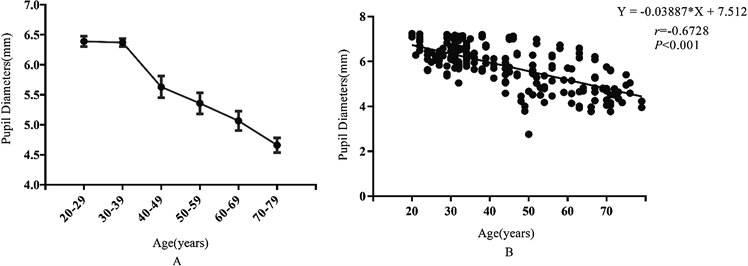
Figure 1. The relationship between the pupil diameters and age ((A) The trend analysis of age and pupil diameters; (B) The correlation between age and pupil diameters)
图1. 年龄与瞳孔直径的关系((A) 年龄与瞳孔直径的趋势分析;(B) 年龄与瞳孔直径的相关性分析)
2、全、前角膜球面像差与年龄的相关性分析
实测全球差和实测前球差趋势相同,均随着年龄的增长而减小,两者呈负相关(r = −0.3323, P < 0.001; r = −0.3703, P < 0.001) (见图2(A),图2(B));理论全球差与年龄无相关性(r = 0.0222, P = 0.756) (见图2(C)),而理论前球差随着年龄增长而增加,呈正相关(r = 0.3551, P < 0.001) (见图2(D))。

Figure 2. The correlation analysis of TCSA and ACSA with age ((A) The analysis of measured TCSA and age; (B) The analysis of measured ACSA and age; (C) The analysis of theoretical TCSA and age; (D) The analysis of theoretical ACSA and age)
图2. 全、前角膜球面像差与年龄的相关性分析((A) 实测全球差与年龄的相关性分析;(B) 实测前球差与年龄的相关性分析;(C) 理论全球差与年龄的相关性分析;(D) 理论前球差与年龄的相关性分析)
3、实测全球差和理论全球差的比较
在E、F组,实测全球差显著低于理论全球差(P < 0.05);其余组中两者间无统计学差异(P > 0.05) (见表1)。

Table 1. Comparison between measured and theoretical TCSA in different age groups
表1. 各年龄段全角膜实测球差和理论球差的比较
4、实测前球差和理论前球差比较
在A组,实测前球差显著高于理论前球差(P < 0.05),在E、F组中,实测前球差显著低于理论前球差(P < 0.05);其他组间两者间无统计学差异(P > 0.05) (见表2)。

Table 2. Comparison between measured and theoretical ACSA in different age groups
表2. 各年龄段前角膜实测球差和理论球差的比较
5、不同年龄段全、前角膜实测和理论球面像差的差异
在20~29、30~39年龄段, 实测全球差显著低于实测前球差(t = −3.736,P = 0.001;t = −6.150,P < 0.001),在70~79年龄段则前者显著高于后者(t = 2,613, P = 0.016),其余年龄段无显著性差异(P > 0.05) (见图3(A))。在30~39,40~49及60~69年龄段,理论全球差著低于理论前球差(t = −3.369,P = 0.001;t = −2.366,P = 0.026;t = −2.596,P = 0.015),其余年龄段无显著性差异(P > 0.05) (见图3(B))。
4. 讨论
像差的概念广泛应用于眼科临床工作中,其中球面像差(以下简称“球差”)是对视觉质量影响很大且唯一可进行有针对性矫正的高阶像差 [11] [12] [13],其主要由角膜球差和眼内球差(一般是晶状体球差)构成。绝大多数正常角膜存在正球差,在不同年龄段较为稳定,年轻时晶状体多为负球差,中和角膜正球差并保持着眼球整体球差平衡 [14] [15]。而晶状体随着年龄增长逐步转变为正球差,人眼总球差增大,导致视网膜成像质量下降 [16]。晶状体摘除后眼球球差主要为角膜球差,此时选择抵消不同程度正球差的消球差人工晶状体类型将影响术后总球差值,因此术前对角膜球差的评估日益受到重视 [17]。
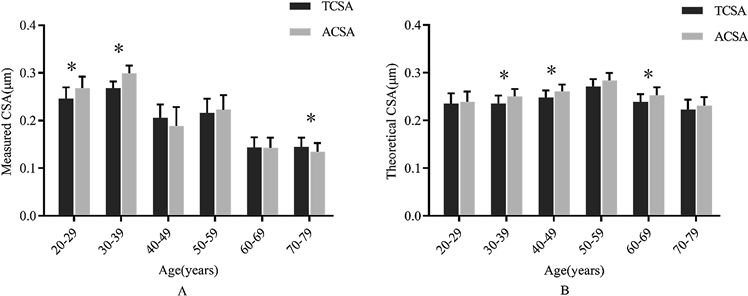
Figure 3. The difference between TCSA and ACSA in every age group. ((A) The difference between measured TCSA and ACSA with age; (B) The difference between theoretical TCSA and ACSA with age. *P < 0.05)
图3. 不同年龄段全、前角膜球面像差的差异((A) 不同年龄段全、前角膜实测球面像差的差异;(B) 不同年龄段全、前角膜理论球面像差的差异。*表示P < 0.05)
目前有很多设备可用于测量角膜球差,如基于Placido环原理的iTrace、OPD光程差分析仪等,只能测量角膜前表面球差。而基于Scheimpflug照相技术的Pentacam、Sirius三维眼前节分析仪等,则可以测量全角膜球差。上述设备均以角膜中央6.0 mm区域球差为默认输出值。Sirius眼前节分析系统同时具备Placido环和Scheimpflug照相技术,可以测量2.0~8.0 mm (以0.5 mm为间隔)范围内的前和全角膜球差,并可以测量3种不同照明环境(模拟白天、黄昏和晚上)下的瞳孔大小 [18] [19]。由于球面像差主要是在暗环境瞳孔扩大状态下影响视觉质量,所以我们主要测量模拟暗环境下(0.4 xl)的实际瞳孔直径。
本研究发现,实测瞳孔直径随年龄的增大而缩小,呈负相关关系。中老年人群,暗环境下实测平均瞳孔直径小于6.0 mm,将基于此瞳孔直径下的球差作为默认输出值将与实际不符,且年龄越大,偏离越大。不论是全角膜球差还是前角膜球差,在60岁以上人群,根据实测瞳孔直径拟合所得实测球差显著低于基于6.0 mm瞳孔直径所得理论球差值,针对这一人群如仍依据理论球差选择消球差非球面人工晶状体类型,将造成术后全眼球差与偏离预期。
角膜前表面生物参数的测量是将角膜表面模拟为一个二维面薄透镜进行分析,而真实的角膜是呈前、后表面双曲面形态并有一定厚度,是作为一个厚透镜存在。不仅仅角膜前表面会影响光学折射,后表面同样也会对折射产生影响,继而对像差产生影响,故采用全角膜参数比单纯使用前表面参数更接近真实状态。既往认为大多数情况下角膜前表面像差可以代表角膜全表面像差 [19],但年龄和个体的差异可能造成部分患者不符合这个规律。
朱柯柯 [20] 等人发现全角膜球差和角膜前表面球差与年龄呈正相关。本研究发现,在6.0 mm瞳孔直径下,理论全球差与年龄无线性关系,在各年龄组间同样无差异,而理论前球差则随年龄增长呈升高趋势,青年人群显著低于中、青年人群,在部分年龄段(30~49,60~69年龄段),全角膜理论球差也低于前角膜理论球面像差;在实测瞳孔直径下,实测全球差和实测前球差虽然均随年龄的增长而减小,但其在人群中分布不同,老年群体实测全球差显著低于青、中年人群,青年人群的实测前球差则高于中老年群体,在30~39,40~49,60~69年龄段,实测全球差值显著低于实测前球差。可见,无论是6.0 mm还是实测瞳孔直径下,全角膜球差和前角膜球差不同年龄段皆存在明显差异,前角膜球差和全角膜球差不能代替使用。
综上,高年龄段人群是白内障的高发人群,其实测平均瞳孔直径偏离6.0 mm较多,实测全和前角膜球差均与6.0 mm瞳孔直径下数据不符。同时在相同瞳孔直径下,全和前角膜球差数据也存在差异,故我们推荐使用实测瞳孔直径下的全角膜球面像差值作为选择球差人工晶状体的类型的依据。当然,在球差检测中可能还存在Kappa角、瞳孔中心位移、瞳孔规则性等因素的影响,这些尚需进一步的研究来明确。