摘要: 目的:探讨消化道柿石症的临床特点、诊治及治疗方法。方法:回顾性分析我科自2017年1月~2020年1月收治消化道柿石症患者70例。结果:70例患者均行CT检查,66例(94.3%)可见阳性结果。34例(48.57%)患者经药物治疗或内镜治疗成功粉碎柿石并排出。36例(51.43%)患者因无法排出柿石者行手术治疗。结论:既往腹部手术史是影响柿石形成和排出的重要因素,老年人更易出现柿石症。腹部CT安全、无痛、全面,是诊断消化道柿石症的优选方法,药物、内镜治疗柿石安全可靠,但要严格把握手术指征。
Abstract:
Objective: To investigate the clinical features, diagnosis, treatment and treatment of digestive tract persimmon disease. Methods: Retrospective analysis was performed on 70 patients with digestive tract persimmon disease admitted to our department from January 2017 to January 2020. Results: CT examination was performed in all 70 patients, and positive results were found in 66 patients (94.3%). Thirty-four patients (48.57%) were successfully crushed persimmon stone and discharged after drug therapy or endoscopic therapy. 36 patients (51.43%) were treated by surgery, because they could not discharge persimmon stone. Conclusion: Previous abdominal surgery was an important factor affecting the formation and discharge of Persimmon stone, and the elderly were more likely to have persimmon stone syndrome. Abdominal CT is safe, painless and comprehensive, which is the preferred method for the diagnosis of digestive tract persimmon stone. Drug and endoscopic treatment of persimmon stone is safe and reliable, but the surgical indications should be strictly grasped.
1. 介绍
消化道柿石症通常是指患者经口进食柿子、山楂或黑枣等食物后,其在胃中潴留,以其为核心发生物理、化学反应而形成的硬质团块。临床上常表现为上腹部饱胀不适、腹痛,可伴有恶心、呕吐,如诊治不及时可继发肠梗阻、穿孔、溃疡、出血等并发症 [1]。目前治疗方法以内镜、药物、手术治疗为主。我科自2017年1月~2020年1月收治消化道柿石症患者70人入院,现分析报道如下。
2. 临床资料
2.1. 一般资料
本组研究中共收录患者70例,纳入标准为患者腹痛等症状出现前有经口进食柿子、山楂或黑枣等食物的病史。排除标准为患者无上述病史,或者考虑其他原因所致腹痛等症状。一般资料见表1。查体腹部均有压痛,15例患者可触及腹部包块。70例患者均行CT检查,66例(94.3%)可见胃内或肠道内类圆形或椭圆形混杂密度团块,团块内可见不均匀气泡影,部分患者肠内可见气液平。39例(55.7%)患者行胃镜诊治,38例(54.3%)在胃内可见质硬柿石,其中1例行胃镜柿石已进入十二指肠,胃镜未见柿石。本研究涉及的所有患者临床资料均患者本人书面知情同意,青岛大学附属医院伦理委员会批准本项研究。
2.2. 治疗方法与结果
所有患者收入院后均给予禁饮食、持续胃肠减压、抑酸保胃、生长抑素微量泵入、预防腹腔感染、静脉补液等对症治疗。完善检查后行内镜下机械碎石。34例(48.57%)患者经药物治疗或内镜治疗成功粉碎柿石并排出。36例(51.43%)患者因无法排出柿石者行手术治疗。1周后复查全腹CT平扫均未见柿石。

Table 1. General condition of 70 patients with persimmon stone disease
表1. 70例柿石症患者一般情况
3. 讨论
消化道柿石症多由于进食柿子、山楂或黑枣等富含鞣酸、树胶、果胶、矢布醇的食物,其中鞣酸遇到胃酸可与食物中的蛋白质结合,形成不溶的鞣酸蛋白而沉淀于胃内,而果胶和树胶遇酸形成凝胶,将沉淀的鞣酸蛋白粘合成块,并与食物纤维残渣凝集形成大小不等的结石 [2]。此外,已确定有多种危险因素与柿石形成有关 [3],如胃肠道手术史 [4]、影响胃肠蠕动的慢性疾病如糖尿病 [5] 等。
我们认为计算机断层扫描(CT)是影像学的优先选择,其灵敏度高达95%和特异度高达70%。CT可以发现消化道内各部位的多种粪石,清楚显示肠袢(绞窄、水肿、缺血、腹腔内积液),并可以准确评估手术指征 [6]。在CT下柿石情况通常表现为:外观为带气泡的圆形或卵圆形团块,其内可见不规则筛状气泡影,边界清楚、边界硬化,呈细线状壳样高密度影,形似胶囊壁,有学者称之为胶囊征(如图1(A)、图1(B));如并发肠穿孔、梗阻可见腹腔游离气体、肠管内气液平等。
柿石的治疗主要取决于其组成成分、体积大小、嵌顿或卡压的位置。治疗方法主要包括:药物治疗,内镜下治疗、手术治疗等。有研究认为质子泵抑制剂、碳酸氢钠、可乐和酶制剂(如胰酶、纤维素酶、木瓜蛋白酶)等均可以对植物性柿石有溶解作用 [7] [8] [9] [10],但具体应用方法、剂量尚未达成共识。可乐是目前最常用的溶解植物性柿石的化学药剂。Ladas等的研究认为可乐对植物性柿石的敏感性高达91%,因此其建议用经鼻胃管注入或经口服用3 L可乐溶解柿石 [10]。但是,如患者合并高龄、糖尿病、溃疡、穿孔等情况时大量可乐可加重病情。另外,溶解后的柿石碎块仍有阻塞幽门、小肠的可能,导致继发性肠梗阻 [11]。因此,需要更多研究来完善和评估药物治疗。
柿石常见位于胃内,因此有些研究推荐内镜下碎石应优先于手术治疗 [12]。在内镜直视下通过活检钳、鼠咬钳、异物钳、鳄鱼嘴钳及息肉圈套等器械,采取抓、割、切等物理方法碎石,粉碎后的柿石碎块可以通过篮网取出、或经消化道排出。内镜下碎石局限性较大,仅适用于胃内的、质地较软、直径较小的柿石,对于质地坚硬、位置低于幽门、直径较大的柿石治疗效果欠佳(如图2)。另外,内镜下碎石的专门器械非内镜室常规配置,多数地区和医院尚未配备,价格高昂,且易损耗,医疗成本较大。
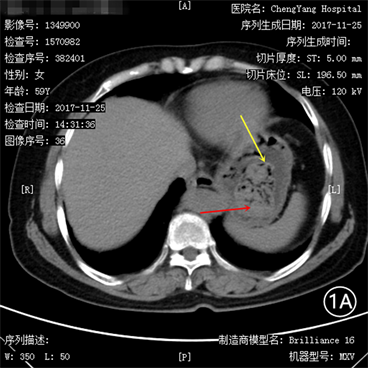
Figure 1. (A) A huge mixed-density mass in the stomach with irregular sieve or honeycomb-shaped air bubbles (red arrow); its boundary is clear and the edges are hardened, also known as the “capsule sign” (yellow arrow); (B) Large mixed density clumps in the intestine, with irregular sieve-shaped or honeycomb-shaped air bubbles (red arrows); clear borders and hardened edges, also known as “capsule sign” (yellow arrows); combined intestinal obstruction can be seen Multiple intestinal gas and liquid level (green arrow)
图1. (A)胃内巨大混杂密度团块,其内见不规则筛状或蜂窝状气泡影(红色箭头);其边界清楚、边缘硬化,又称“胶囊征”(黄色箭头);(B):肠内巨大混杂密度团块,其内见不规则筛状或蜂窝状气泡影(红色箭头);其边界清楚、边缘硬化,又称“胶囊征”(黄色箭头);合并肠梗阻可见多发肠内气液平(绿色箭头)
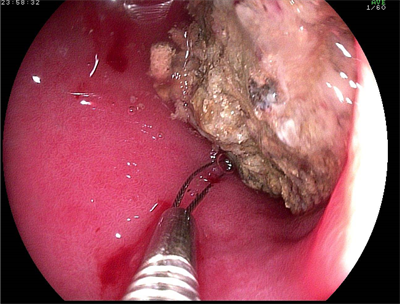
Figure 2. Huge, hard gastrolith in the duodenum under endoscope
图2. 内镜下十二指肠内巨大、坚硬胃石
本次研究中,我们按既往腹部手术史将患者分为既往手术组45例和非手术组25例,既往手术组中34例(75.56%)因保守治疗效果欠佳行手术治疗,非手术组中仅2例(8%)行二次手术治疗,差异明显,说明腹部手术史是影响柿石形成和排出的重要因素之一,这可能与手术会使原解剖结构改变,形成肠粘连,导致肠内容物难排出困难有关;此外,从统计数据中可以发现,老年人更加容易引起柿石症。如诊治过程中腹痛持续不缓解甚至进行性加重,并发腹膜炎、消化道穿孔、消化道出血、肠扭转、肠梗阻、腹水等并发症者,需急症手术干预。另外,如果柿石通过幽门后,进入空肠、回肠,药物溶石和内镜碎石效果均欠佳,则需手术治疗。随着技术不断发展,腹腔镜手术逐步成为主流,柿石症是否发生率会降低,有待未来进一步研究。手术方案通常是剖开肠管取出柿石,也有推荐通过挤压的方法将柿石粉碎后向远端肠管推进,最好将柿石及(或)碎块推至通过回盲瓣。但是这样做易导致肠浆膜层、肠系膜撕裂,也有可能并发黏膜出血。因此手术方案选择需谨慎,操作过程需轻柔,如预计方案无法顺利进行,及时调整手术方法。
4. 结论
综上所述,我们认为,对于柿石症患者应首先详细询问病史、完善全腹CT检查,明确柿石大小、位置,病程早期可优先考虑药物治疗,治疗过程中完善内镜检查、定期复查全腹CT,评估手术指征,对前述治疗方案效果较差者或合并急性并发症者及时采取手术治疗。
致谢
感谢国家自然科学基金资助项目(项目编号:50902110)。
NOTES
*通讯作者。