摘要:
目的:探讨原发性硬脑膜低级别B细胞边缘区淋巴瘤的临床及影像学表现。方法:回顾性分析5例经手术与病理证实的原发性硬脑膜低级别B细胞边缘区淋巴瘤的临床表现及影像学特征。结果:共5例患者,其中男性1例,女性4例。年龄45~69岁,平均年龄54岁,中位年龄54岁。5例(100%)患者均有头痛,2例(40%)癫痫,2例(40%)肢体无力,1例(20%)恶心,1例(20%)言语不能,1例(20%)视野缺损。5例患者病变均位于颅板下硬脑膜。3例(60%)呈新月形,1例(20%)呈双凸透镜形,1例(20%)呈匍匐形。5例(100%)与脑实质呈等密度,边界不清。病变最大者最大截面约75 mm × 12 mm,最小者病变最大截面约17 mm × 4 mm。4例(80%)可见邻近颅骨不同程度骨质破坏。T1WI稍低信号3例(60%),等信号2例(40%);T2WI稍高信号5例(100%);T2-FLAIR稍高信号5例(100%);DWI稍高信号4例(80%),等信号1例(20%);5例(100%)均明显强化,脑实质呈受压推移改变。结论:原发性硬脑膜淋巴结较为罕见,在影像上容易被误诊为硬膜下血肿等。接受正确的诊断与治疗,病人预后较好,所以当临床与影像表现不符时,将其纳入鉴别诊断是及其重要的。
Abstract:
Objective: To investigate the clinical and imaging manifestations of primary dural lymphoma. Methods: The clinical manifestations and imaging features of 5 cases of primary dural low-grade B-cell marginal zone lymphoma confirmed by operation and pathology were analyzed retrospectively. Results: There were 5 patients, including 1 male and 4 females. The age ranged from 45 to 69 years old, the average age was 54 years old, and the median age was 54 years old. All 5 (100%) patients had headache, 2 (40%) epilepsy, 2 (40%) limb weakness, 1 (20%) nausea, 1 (20%) speech disability and 1 (20%) visual field defect. The lesions of 5 patients were located in the subcranial dura mater. 3 cases (60%) were crescent-shaped, 1 case (20%) was biconvex lens, and 1 case (20%) was creeping. 5 cases (100%) were isodensity with brain parenchyma, and the boundary was not clear. The maximum cross section of the largest lesion was about 75 mm × 12 mm, and the maximum cross section of the smallest lesion was about 17 mm × 4 mm. Different degrees of bone destruction of the adjacent skull could be seen in 4 cases (80%). T1WI slightly low signal in 3 cases, iso-signal in 2 cases, T2WI slightly high signal in 5 cases, T2-FLAIR slightly high signal in 5 cases (100%); DWI slightly high signal in 4 cases, iso-signal in 1 case, 20%), obvious enhancement in 5 cases (100%), brain parenchyma changed by compression. Conclusion: primary dural lymph nodes are rare and are easily misdiagnosed as subdural hematoma. When patients receive correct diagnosis and treatment, the prognosis is good, so when the clinical and imaging manifestations are not consistent, it is very important to include it in the differential diagnosis.
1. 引言
原发性中枢神经系统淋巴瘤(Primary central nervous system lymphoma, PCNSL)是一种少见的中枢神经系统肿瘤。它们是一组结外非霍奇金淋巴瘤(NHL),主要起源于B细胞 [1]。而原发性硬脑膜低级别B细胞边缘区(粘膜相关淋巴组织,MALT)淋巴瘤是一种罕见的原发性中枢神经系统淋巴瘤亚型,其影像学表现可以与硬膜下血肿、脑膜瘤相似,容易对诊断造成困扰,绝大多数需要根据术后病理检查结果才能够明确诊断 [2]。正确的影像学诊断,可以指导临床治疗,为患者争取一个良好预后。
2. 资料与方法
2.1. 一般资料
收集自2014年1月至2020年4月确诊为原发性硬脑膜低级别B细胞边缘区(粘膜相关淋巴组织,MALT)淋巴瘤患者共5例。其中男性1例,女性4例,年龄45~69岁,平均年龄54岁,中位年龄54岁。
2.2. 检查方法
MRI检查应用GE 1.5T或GE 3.0T超导型磁共振仪。应用头线圈,FSE T2WI (TR 4000 ms, TE 104 ms)、TlWI (TR 2250 ms, TE 7.5 ms, TI 750 ms)、T2-FLAIR (TR 8000 ms, TE 133 ms, TI 2000 ms)及DWI (b = 1000)序列扫描。矩阵320 × 256,FOV:240 mm × 180 mm,层厚5 mm,间隔1.5 mm。5例进行轴、冠状、矢状面MRI增强扫描。
2.3. 影像分析
由3名具有5年以上工作经验的神经影像方向的影像科医师及2名具有5年以上工作经验的神经科医师对病人的影像学资料及临床资料进行综合分析,如有分歧协商达成一致。分析要点包括:肿瘤的位置(额部、顶部、颞部、枕部、颅底),大小(最大截面测量肿块的长度、宽度),形态(匍匐生长呈新月形、双面凸起呈凸透镜形),密度及信号特点,硬脑膜及软脑膜累及情况,脑实质受累情况,颅骨骨质改变及增强扫描后肿块强化程度。
3. 结果
3.1. 原发性硬脑膜低级别B细胞边缘区淋巴瘤的临床表现
共5例患者,其中男性1例,女性4例。年龄45~69岁,平均年龄54岁,中位年龄54岁。5例(100%)患者均有头痛,2例(40%)癫痫,2例(40%)肢体无力,1例(20%)恶心,1例(20%)言语不能,1例(20%)视野缺损,如表1所示。

Table 1. Summary of the main clinical characteristics of the patients in this study
表1. 本研究中患者的主要临床特点
3.2. 原发性硬脑膜低级别B细胞边缘区淋巴瘤的CT表现
本组5例患者病变均位于颅板下硬脑膜。3例(60%)呈新月形,1例(20%)呈双凸透镜形,1例(20%)呈匍匐形。5例(100%)与脑实质呈等密度,边界不清。病变最大者最大截面约75 mm × 12 mm,最小者病变最大截面约17 mm × 4 mm。4例(80%)可见邻近颅骨不同程度骨质破坏,如表2及图1所示。

Table 2. Summary of the main CT characteristics the patients in this study
表2. 本研究中患者的主要CT特征
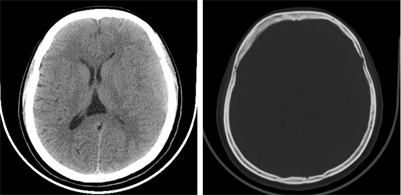
Figure 1. The patient is a 47-year-old woman. CT scan showed isodensity mass shadows in the left frontotemporal region, with unclear boundaries and lytic bone destruction in adjacent bones
图1. 患者女性,47岁。CT平扫示左侧额顶颞部等密度肿块影,边界不清,邻近骨质呈溶骨性骨质破坏
3.3. 原发性硬脑膜低级别B细胞边缘区淋巴瘤的MR表现
5例患者中,T1WI稍低信号3例(60%),等信号2例(40%);T2WI稍高信号5例(100%);T2-FLAIR稍高信号5例(100%);DWI稍高信号4例(80%),等信号1例(20%);5例(100%)均明显强化,可见脑膜尾征,脑实质呈受压推移改变,如表3及图2所示。

Table 3. Summary of the main MR characteristics the patients in this study
表3. 本研究中患者的主要MR特征
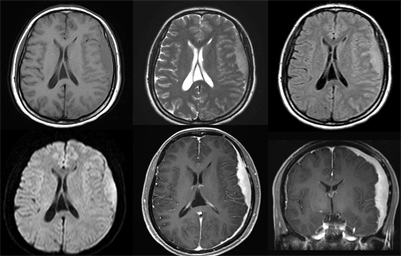
Figure 2. MR manifestations of the same patient: slightly low signal on T1WI, slightly high signal on T2WI, slightly high signal on T2-FLAIR, and slightly high signal on DWI. Contrast-enhanced scan showed significant enhancement, with meningeal cauda sign
图2. 同一患者MR表现:T1WI呈稍低信号,T2WI呈稍高信号,T2-FLAIR呈稍高信号,DWI呈稍高信号。增强扫描可见明显强化,见脑膜尾征
3.4. 病理表现
本组5例患者均行手术治疗。术后巨检,5例肿瘤均呈肿物色灰,质软,血供丰富。镜下检查:肿瘤内见淋巴组织增生性病变,散在残留大小不一的淋巴滤泡,滤泡间小淋巴样细胞呈弥漫性分布,细胞大小较一致,形态单一,如图3所示。免疫组化结果:CD3 (−) 5例,CD20 (+) 5例,CD79a (+) 4例,CD10 (−) 5例,Bcl-6 (−) 3例,Bcl-2 (+) 4例,CD21示滤泡树突网,CyclinD1 (−) 5例,CD5 (−) 3例,CD23 (−) 5例,Ki-67阳性率约30% 3例,20% 2例。进一步行IGH、IGK、IGL重排克隆性分析以鉴别诊断,使用欧洲BIOMED-2方案和ABI3500DX型基因测序仪对标本基因组DNA中IGH、IGK、IGL重排的克隆性进行分析检测结果:IGH-A:阳性5例,IGH-B:阴性3例,IGH-C:阴性4例,IGH-D:阴性4例,IGH-E:阴性5例,IGK-A:阴性4例,IGK-B:阴性5例,IGL:阴性5例。IG重排阳性主要见于淋巴细胞增殖性疾病。在B细胞肿瘤中IGH阳性率为80%,IGK阳性率为90%,两者同时检测阳性率 > 95%。IGL基因重排阳性是对IGK基因重排的补充和验证。结合镜下形态、免疫组化及IG基因重排检测结果,考虑5例均为低级别B细胞边缘区(粘膜相关淋巴组织,MALT)淋巴瘤。
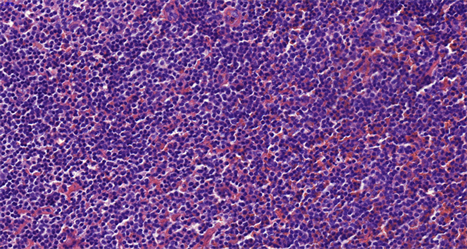
Figure 3. At 400 magnification, proliferative lesions of lymphoid tissue were found in the tumor, scattered in the residual lymphoid follicles of different sizes. Small lymphoid cells were distributed diffusely between follicles, with uniform cell size and single morphology
图3. 放大400倍镜下肿瘤内见淋巴组织增生性病变,散在残留大小不一的淋巴滤泡,滤泡间小淋巴样细胞呈弥漫性分布,细胞大小较一致,形态单一
4. 讨论
中枢神经系统内的淋巴瘤可继发于全身性疾病,原发性中枢神经系统淋巴瘤较为罕见。原发性中枢神经系统淋巴瘤是一种罕见的结外型非霍奇金淋巴瘤,约占非霍奇金淋巴瘤的1%~2%。原发性中枢神经系统淋巴瘤约占中枢神经系统肿瘤的2%~4% [3]。
原发性硬脑膜淋巴瘤是一种罕见的原发于硬脑膜而非脑实质的中枢神经系统淋巴瘤,在生物学上不同于其他中枢神经系统淋巴瘤 [4]。通常为低级别淋巴瘤,颅内边缘区B细胞淋巴瘤(MALT)是原发于中枢神经系统淋巴瘤的一种罕见的亚型,常发生于硬脑膜及侧脑室脉络丛。
原发性硬脑膜淋巴瘤的发病率尚不清楚,多见于中年妇女 [5] [6]。移植术后、或患有获得性免疫缺陷综合征、胶原血管等疾病的免疫功能低下的患者,发生此类肿瘤的概率较高 [7] [8]。本组患者4例为女性,与文献报道相符,但本组患者无上述疾病病史。由于硬脑膜不含任何淋巴组织,原发性硬脑膜淋巴瘤的发病机制尚不清楚,原发性颅内淋巴瘤是如何在缺乏淋巴系统的硬脑膜中发展而来仍有待探究。有文献表明,外周B细胞的恶性转化将被免疫系统识别和消灭,然而在中枢神经系统中免疫功能减弱,抗肿瘤免疫反应可能不足,导致了原发性中枢神经系统淋巴瘤的发生 [9] [10]。
头痛和癫痫是硬脑膜淋巴瘤最常见的症状。然而,根据它们的大小和位置,可以引起相应的临床症状和体征。本组患者5例(100%)患者均有头痛,2例(40%)癫痫,2例(40%)肢体无力,1例(20%)恶心,1例(20%)言语不能,1例(20%)视野缺损。目前,硬脑膜淋巴瘤尚无明确的治疗和管理方案。大多数患者接受手术切除、放疗、化疗或上述治疗方式的联合治疗。总的来说,这种惰性肿瘤通常预示着一个良好的结果。
原发性硬脑膜淋巴瘤在影像学上通常表现为以脑膜为基底生长类似于脑膜瘤的肿块 [11]。本组病例MRI多表现为T1WI呈稍低信号、T2WI呈稍高信号,T2-FLAIR及DWI均呈稍高信号,信号均匀,未见明显出血及钙化,增强扫描后肿瘤整体均匀强化,可见脑膜尾征。CT平扫病灶呈稍高密度,骨窗可见临近颅板呈溶骨性破坏。
原发性硬脑膜低级别B细胞边缘区(粘膜相关淋巴组织)淋巴瘤的鉴别诊断:1) 硬膜下血肿:CT平扫表现与硬脑膜淋巴瘤相似,但患者多有颅脑外伤史,短期复查可见血肿密度降低,范围减小,且无骨质破坏。如有虫蚀样骨质破坏,且复查病变未吸收,应考虑硬脑膜淋巴瘤的可能性,及时行MR检查及活检,以免延误治疗时机。2) 脑膜瘤:常可见钙化,而硬脑膜淋巴瘤无钙化。脑膜瘤往往为成骨性改变,溶骨性骨质破坏少见。但硬脑膜淋巴瘤早期便侵犯周围骨质,在CT骨窗及MR增强上容易观察。脑膜瘤其脑膜尾征一般从肿瘤向外逐渐变细,边界光整,脑膜尾征强化程度往往比肿瘤本身更为明显。而硬脑膜淋巴瘤的脑膜尾征并无此表现。少数脑膜瘤可见放射状血管流空的低信号影,而MALT淋巴瘤于增强图像上可见放射状强化信号影。3) 血管周细胞瘤:男性较女性多发。一般病灶体积较大,边缘多见分叶,血供丰富。生长速度快,内部多见坏死、出血及囊变,信号不均,增强扫描呈明显不均匀强化。易复发及转移。
综上所述,即便是面对免疫功能正常的患者,临床医师也应注意将原发性硬脑膜淋巴瘤纳入硬脑膜病变的鉴别诊断之中,早诊断早治疗,为病人争取一个良好预后。
参考文献