摘要: 目的:探讨CA19-9、中性粒细胞淋巴细胞比率(NLR)、血小板淋巴细胞比率(PLR)、单核细胞淋巴细胞比率(MLR)和全身免疫炎症指数(SII)在肝外胆管癌(ECC)中的诊断价值。方法:选取2012年1月~2021年9月青岛市市立医院收治的ECC患者150例作为ECC组及150例健康体检者作为对照组,对其CA19-9、NLR、PLR、MLR和SII进行检测分析。采用受试者工作特征(ROC)曲线分析各指标单独和联合检测诊断ECC的效能。结果:ECC组CA19-9、NLR、PLR、MLR、SII的水平均高于对照组(P < 0.05)。ROC曲线分析显示,CA19-9、NLR、PLR、MLR、SII诊断ECC所对应的AUC值分别为0.899、0.869、0.857、0.796、0.884,四项炎症指标诊断敏感性分别为68.70%、74.00%、72.70%、79.30%,特异性分别为94.00%、84.00%、76.00%、87.30%,CA19-9联合四项炎症指标进行诊断的AUC值为0.975,敏感性和特异性为92.00%和96.70%。结论:CA19-9、NLR、PLR、MLR、SII在ECC患者中升高,对于ECC的诊断有一定价值,联合诊断相比于单个指标具有更高的诊断效能。
Abstract:
Objective: To investigate the diagnostic value of CA19-9 combined with neutrophil lymphocyte ratio (NLR), platelet lymphocyte ratio (PLR), monocyte lymphocyte ratio (MLR) and systemic immune inflammation index (SII) in extrahepatic cholangiocarcinoma (ECC). Methods: 150 patients with ECC treated in Qingdao Municipal Hospital from January 2012 to September 2021 were selected as the cholangiocarcinoma group and 150 healthy patients as the control group. CA19-9, neutrophil lymphocyte ratio (NLR), platelet lymphocyte ratio (PLR), monocyte lymphocyte ratio (MLR) and systemic immune inflammation index (SII) were detected and analyzed. The diagnostic efficiency of single and combined parameters for ECC was evaluated by the ROC (receiver operating characteristic) curve. Results: The levels of CA19-9, NLR, PLR, MLR and SII in ECC group were higher than those in control group (P < 0.05). The ROC curve analysis showed that the areas under the ROC curve corresponding to the diagnosis of ECC by CA19-9, NLR, PLR, MLR and SII were 0.899, 0.869, 0.857, 0.796 and 0.884 respectively. The diagnostic sensitivity of NLR, PLR, MLR and SII was 68.70%, 74.00%, 72.70% and 79.30% respectively, and the specificity was 94.00%, 84.00%, 76.00% and 87.30% respectively. The area under the curve of CA19-9 combined with NLR, PLR, MLR and SII was 0.975, and the sensitivity and specificity were 92.00% and 96.70%. Conclusion: CA19-9, NLR, PLR, MLR and SII are increased in patients with ECC, which is of certain value for the diagnosis of ECC. Combined diagnosis has higher diagnostic efficiency than single index.
1. 引言
胆管癌(Cholangiocarcinoma, CCA)是一种起源于胆管上皮细胞的胆道系统恶性肿瘤,是消化系统中罕见的恶性肿瘤之一,根据其解剖位置可分为肝内、肝门部和远端胆管癌,其中肝门部和远端胆管癌又统称为肝外胆管癌(extrahepatic cholangiocarcinoma, ECC) [1]。ECC的预后普遍较差,据统计,ECC术后中位生存时间为19个月,5年生存率仅4% [2]。因缺乏敏感和特异的生物标志物,大多数CCA病例是在晚期发现的。CA19-9是目前临床最常用的诊断ECC的生物标志物,然而,血清CA19-9在诊断上缺乏特异性和敏感性 [3]。最近的研究表明,炎症相关的外周细胞,如中性粒细胞、血小板和淋巴细胞,与肿瘤的进展、转移和免疫反应显著相关 [4]。中性粒细胞淋巴细胞比率(neutrophil lymphocyte ratio, NLR)、血小板淋巴细胞比率(platelet lymphocyte ratio, PLR)、单核细胞淋巴细胞比率(monocyte lymphocyte ratio, MLR)是几种常见的炎症指标,与肿瘤密切相关 [5] [6] [7]。全身免疫炎症指数(systemic immune-inflammation index, SII)作为NLR与血小板计数的结合,其作用可能优于单一的炎症指标 [8]。本研究通过探讨CA19-9、NLR、PLR、MLR、SII在ECC诊断中的价值,以及它们联合诊断的意义,以期为ECC早期诊断和评估提供有力数据。
2. 资料与方法
2.1. 一般资料
收集2012年1月~2021年9月在青岛市市立医院收治的ECC患者150例作为胆管癌组及150例健康体检者作为对照组。纳入标准:经术后病理证实为胆管恶性病变。排除标准:①合并其他组织器官肿瘤;②基础疾病如高血压、糖尿病及心血管疾病等较多且合并严重感染、免疫系统疾病等;③合并血液系统疾病或血常规异常者等。本研究通过本院伦理委员会审批且受试者同意并签署相关知情同意书。其中胆管癌组男108例,女42例;平均年龄(54 ± 12)岁。对照组男107例,女43例;年龄(51 ± 10)岁。两组间性别、年龄比较差异无统计学意义(P > 0.05),具有可比性。
2.2. 方法
收集受试者一般资料及实验室检查结果,包括患者初次入院的血常规及CA19-9检测结果,根据血常规结果计算出NLR、PLR、MLR、SII。CA19-9使用雅培i2000化学发光仪检测,血常规采用SYSMEX全自动血细胞分析仪检测。
2.3. 分析方法
运用SPSS 25和GraphPad Prism 9进行数据处理分析。符合正态分布的计量资料以(
)表示,组间比较用独立样本t检验;非正态分布计量资料以[M(P25, P75)]表示,组间比较用Mann-Whitney U检验。采用受试者工作特征(ROC)曲线对血清CA19-9、NLR、PLR、MLR、SII进行诊断分析,以Logistic回归对上述指标联合诊断进行综合分析。均以P < 0.05为差异有统计学意义。
3. 结果
3.1. ECC组和对照组CA19-9、NLR、MLR、PLR、SII的比较
ECC组CA19-9、NLR、PLR、MLR、SII的水平均明显高于对照组,差异有统计学意义(P < 0.05),见图1,表1。
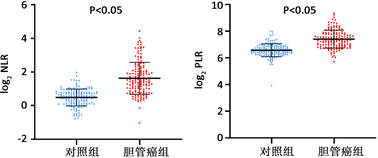
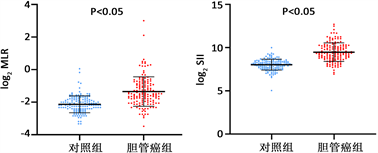 注:纵坐标以log2表示。
注:纵坐标以log2表示。
Figure 1. Comparison of NLR, PLR, MLR and SII between ECC group and control group
图1. 胆管癌组和对照组NLR、MLR、PLR、SII的比较

Table 1. Comparison of clinical data between ECC group and control group
表1. 胆管癌组与对照组临床资料比较
3.2. CA19-9、NLR、PLR、MLR、SII对ECC的诊断效能
对上述指标诊断效能运用ROC曲线分别进行分析,CA19-9、NLR、PLR、MLR、SII均呈现了较高的ECC的诊断性能,曲线下面积(AUC)分别为0.899、0.869、0.857、0.796、0.884,其中CA19-9的诊断效能最高。根据约登指数将CA19-9的Cut-off值设为25 U/ml时,其敏感性仅为85.30%,然而联合其余四项指标时可以显著提高ECC的诊断效能(AUC = 0.975),敏感性和特异性分别可以达到92.00%和96.70%,且差异有统计学意义(P < 0.05)。NLR、PLR、MLR、SII的约登指数对应最大截断值分别为2.19、125.15、0.29、403.37,见表2,图2。

Table 2. Efficacy of CA19-9, NLR, PLR, MLR, SII in the diagnosis of ECC
表2. CA19-9, NLR, PLR, MLR and SII对ECC诊断效能的分析
4. 讨论
胆管癌由于其非特异性症状、大多数诊断方法的敏感性和特异性低以及缺乏绝对诊断标准而难以诊断。因此,对临床医生来说,及时诊断胆管癌有时是一项具有挑战性的任务。CA19-9是目前应用最广泛的用于胆管癌早期筛查的肿瘤标志物,对胆管癌的诊断和病情监测有一定的意义,但敏感性不强。大型荟萃分析表明,血液CA19-9诊断胆管癌,其敏感性和特异性分别为72%和84% [9]。因此需要联合检测,才能提高可靠性。
目前,人们广泛认识到全身炎症反应与肿瘤细胞的增殖、侵袭及血管的生成密切相关 [10]。中性粒细胞可以分泌TNF-α、VEGF和白细胞介素,从而促进肿瘤细胞增殖和血管生成;淋巴细胞可以介导细胞

Figure 2. The diagnostic efficiency of single and combined parameters in ECC
图2. 单个指标及联合诊断对ECC的诊断效能
毒性并释放细胞因子,从而表现出抑制肿瘤细胞生长、增殖和转移的抗肿瘤作用;血小板可分泌TGF-β、VEGF和血小板衍生因子,加速分化和肿瘤细胞的增殖,并在肿瘤组织的粘附和血管生成中发挥重要作用 [11]。单核细胞可以分化为肿瘤相关巨噬细胞,从而对肿瘤生长、肿瘤细胞浸润和血管生成产生促进作用 [12]。全身免疫炎症指数(systemic immune-inflammation index, SII)由(N × P)/L计算得到(N、P和L分别代表中性粒细胞计数、血小板计数和淋巴细胞计数),与基于2种类型血细胞的比值(如NLR和PLR)相比,通过3种类型血细胞数量计算得到的SII可能是一种能更均衡反映机体炎症状态的指标 [13]。已有研究表明,PLR和NLR、SII可作为远端胆管癌的术前预后标志物,PLR、NLR、SII是总生存时间(overall survival, OS)独立影响因素 [14] [15] [16]。因此,NLR、PLR、MLR和SII在理论上是预测肿瘤及其预后有价值的生物标志物,并且这些指标都可以很容易地从常规检查中获得。
本研究结果表明,ECC组NLR、PLR、MLR、SII的水平分别为3.96 (0.49, 21.61)、190.49 (52.35, 654.84)、0.52 (0.09, 8.05)、964.78 (123.44, 6657.62),高于对照组的1.49 (0.58, 3.94)、100.78 (15.35, 256.96)、0.25 (0.10, 1.04)、287.28 (32.86, 1027.85),差异有统计学意义(P < 0.05),提示NLR、PLR、MLR、SII有可能成为诊断ECC的辅助指标。ROC曲线分析显示,CA19-9、NLR、PLR、MLR、SII诊断ECC所对应的ROC曲线下面积分别为0.899、0.869、0.857、0.796、0.884,说明它们各自对ECC的诊断具有一定意义。其中NLR、MLR、PLR、SII诊断敏感性分别为68.70%、74.00%、72.70%、79.30%,特异性分别为94.00%、84.00%、76.00%、87.30%,虽低于CA19-9的85.30%和97.30%,但是对于CA19-9在诊断ECC时可能起到补充的作用。分析CA19-9联合NLR、PLR、MLR、SII预测ECC的ROC曲线发现,其对应的曲线下面积可达0.975,在敏感度得到提高的同时,特异度下降不明显,提示联合检测对ECC诊断具有较高的临床价值,从而为ECC的辅助诊断、治疗监测提供参考。
5. 结论
综上所述,CA19-9联合NLR、PLR、MLR、SII对于ECC的诊断有一定价值,敏感性和特异性均较高,但本研究的样本含量相对不足,仍需要大样本的前瞻性研究验证其可靠性,并且可以进一步探讨CA19-9及炎症指标与ECC病理特征的关系。