摘要: 目的:探讨多瘘口骶段硬脊膜动静脉瘘的临床特点,诊断与治疗。方法:结合本院多瘘口骶段硬脊膜动静脉瘘病例,参考国内外文献,处理并分析此类疾病患者的临床症状及表现、体征、腰骶椎MR表现、脊髓血管造影表现、手术方法及预后。结果:患者因“右下肢麻木9月余,加重3月”入院,胸腰椎磁共振检查显示胸髓及腰椎管增粗、脊髓腹侧大量流空影;脊髓血管造影检查显示骶3、骶5水平各有一处瘘口。术后病理脂肪瘤伴血管畸形。结论:骶段多瘘口硬脊膜动静脉瘘病例较为罕见,早期症状不明显且易漏诊,磁共振检查对此病诊断有一定的参考意义,脊髓血管造影术是此病诊断的金标准,首选的治疗措施是外科显微镜下阻断瘘口治疗。
Abstract:
Objective: To investigate the clinical characteristics, diagnosis and treatment of sacral dural arteriovenous fistula with multiple fistulas. Methods: Combined with the cases of multiple fistula sacral dural arteriovenous fistula in our hospital, referring to the domestic and foreign literature, the clinical symptoms and manifestations, physical signs, lumbosacral MR manifestations, spinal cord angiography manifestations, surgical methods and prognosis of patients with this kind of disease were analyzed. Results: The patient was hospitalized because of “numbness of right lower limb for more than 9 months, aggravating for 3 months”. MRI examination of thoracolumbar spine showed that the thoracic spinal cord and lumbar spinal canal were thickened, and a large number of empty shadows were found in the ventral side of spinal cord; spinal angiography showed that there was a fistula at the level of sacral 3 and sacral 5. Postoperative pathological was lipoma with vascular malformation. Conclusion: The cases of sacral multi fistula dural arteriovenous fistula are rare; the early symptoms are not obvious and easy to miss diagnosis. Magnetic resonance examination has a certain reference significance for the diagnosis of this disease. Spinal cord angiography is the gold standard for the diagnosis of this disease, and the first choice of treatment is to block the fistula under surgical microscope.
1. 引言
硬脊膜动静脉瘘(spinal dural arteriovenous fistulas, SDAVF)是脊髓血管畸形的一种,指脊髓前或脊髓后动脉与静脉之间的直接交通,导致逐渐进展的脊髓功能障碍。SDAVF的病因尚未明确,可位于从颈髓到马尾的任何节段,常见T5-7和T12-L3水平。此类病例常起病隐匿,不易早期诊断且易误诊,随着影像学包括MRI、DSA在SDAVF中的应用及发展,此种疾病的发现越来越多 [1]。本文就我科近期收治的1例采用显微镜下外科手术治疗成功的有两个瘘口的SDAVF患者的临床资料及影像学资料进行分析。
2. 病例资料
患者,男性,44岁,汉族,办公室职员,因右下肢麻木9月余,加重3月入院。患者9月余前自感右下肢麻木,无活动不利,无大小便障碍,于外院就诊,行针灸、按摩等保守治疗,效果不佳。3月前右下肢麻木感加重,出现行走不稳症状,行走时间过长或爬楼时加重,休息可缓解,于外院就诊,行胸腰椎MRI示:T1-S3节段脊髓血管畸形。自发病至入院,饮食、睡眠可,大小便无明显异常,体重下降4 Kg。余无特殊病史。
入院查体:发育正常,皮肤粘膜无明显异常,全身浅表淋巴结未及肿大。神经系统查体:右下肢肌力4级,双下肢感觉减退,双侧膝反射(++),双侧跟腱反射(++)。双侧巴氏征及戈登征阴性,无颈项强直,克氏征及布氏征阴性。
胸腰椎MRI示胸1至骶3节段椎管内扩张迂曲的流空血管,脊髓圆锥T2WI高信号改变,T1WI呈等信号,其余节段胸髓信号无明显异常(图1(A)~(D))。



 (A) T2WI胸椎矢状位,胸髓可见增粗,脊髓腹侧大量流空影(箭头);(C) T2WI腰椎矢状位,椎管可见增粗,内可见圆形流空影(箭头)
(A) T2WI胸椎矢状位,胸髓可见增粗,脊髓腹侧大量流空影(箭头);(C) T2WI腰椎矢状位,椎管可见增粗,内可见圆形流空影(箭头)
Figure 1. Preoperative magnetic resonance imaging (MRI)
图1. 术前MRI
入院后结合患者病史有行走不稳,查体右下肢肌力4级,以及胸腰椎影像学表现,初步诊断为脊髓血管畸形,为进一步明确诊断,行脊髓血管造影术。影像分析:左髂内动脉造影显示骶外侧动脉发出增粗分支于第二骶前孔水平入骶管,向上行至腰4锥体下缘后折返,于骶3锥体水平与骶管内静脉直接沟通,对比剂经一条显著增粗迂曲的引流静脉头侧引流(图2(B)、图2(C))。右髂内动脉造影示右臀下动脉远端骶尾部细小分支于骶5锥体下缘与静脉沟通,对比剂经紊乱纤细引流静脉向头端引流至骶3水平后使前述异常引流静脉浅淡显影(图2(F))。符合骶段硬脊膜动静脉瘘血管造影表现(骶3、骶5水平)。
患者骶3、骶5水平硬脊膜动静脉瘘诊断基本明确,下一步行后正中入路脊髓硬脊膜动静脉瘘电灼术+骶管脂肪瘤切除术。取俯卧位,显微镜下探查寻找到S3水平的硬脊膜瘘口(图3),位于左侧S3前口处有1条小动脉与神经伴行进入硬膜下,其远端有迂曲增粗的静脉,电灼并剪断该供血动脉,然后切除S3-5的脂肪瘤并电灼剪断S5水平的供血小动脉。术后给予甲强龙500 mg冲击每天1次连续3天及补液等治疗。术后第三天复查胸腰椎MRI示符合动静脉瘘术后表现,椎管内不规则信号较前明显减少甚至消失(图4),术后病理为脂肪瘤伴血管畸形(图5)。出院后随访,双下肢麻木感明显减轻,无行走不稳,无大小便障碍,无肢体无力。



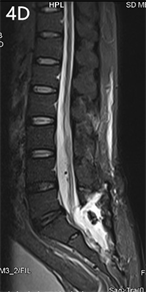 (A)、(B) T2胸椎MRI,流空血管影几乎消失;(C)、(D) T2腰椎MR,圆形血管影明显减少
(A)、(B) T2胸椎MRI,流空血管影几乎消失;(C)、(D) T2腰椎MR,圆形血管影明显减少
Figure 4. Postoperative MRI
图4. 术后MRI
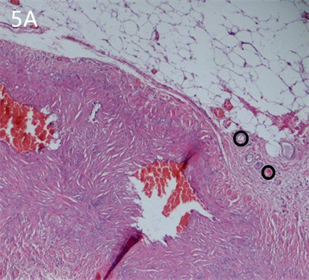
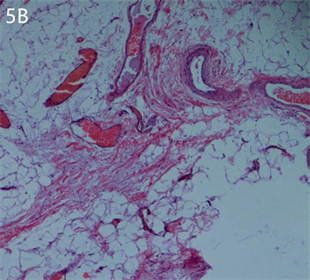 分化成熟的脂肪组织,其内并可见畸形血管,符合脂肪瘤伴血管畸形
分化成熟的脂肪组织,其内并可见畸形血管,符合脂肪瘤伴血管畸形
Figure 5. Pathology (Magnification 10 × 10)
图5. 送检组织病理(放大倍数10 × 10)
3. 讨论
硬脊膜动静脉瘘(spinal dural arteriovenous fistulas, SDAVF)是一种罕见的血管畸形,SDAVF的发病机制尚不清楚,但患者具有相似的特点:多为老年男性患者,瘘常发生在胸段和腰椎段,有缓慢和逐步加重的脊髓下部损伤,被认为与创伤、手术等因素有关,在所有脊柱血管畸形中,SDAVF约占70%,年发病率约为5~10/百万人口 [1]。
本报告中患者为多瘘口硬脊膜动静脉瘘患者,家族中无其他患此类疾病成员。笔者认为,患者的症状、体征及影像学表现对SDAVF有诊断价值,外科手术阻断瘘口动静脉交通是治疗此类疾病的有效手段,若瘘口为多处,术中需找到所有瘘口并予以阻断。
通过影像学的发展,虽然MRI可以用于初步诊断及判断脊髓损伤的严重程度,诊断SDAVF有了长足的进步,但是在此病早期仍然有漏诊或误诊,而且这种疾病仍然没有被完全了解,SDAVF的早期症状通常被错误地归因于神经放射学成像上共存的常见异常,如腰椎管狭窄、椎体前/后移和腰椎间盘突出 [2]。目前证据表明脊随血管造影作为一种有创诊断程序,仍是定位瘘管分流不可缺少的,脊髓血管造影有利于正确的诊断及治疗 [3] [4] [5]。
从国内以及国际上来看,治疗SDAVF有两种主流治疗方式:外科手术治疗和介入栓塞术 [6];两种手术方式的目的相同,阻断瘘口动静脉交通 [7]。早期介入栓塞术复发率达83%,随着介入技术的发展,此治疗方式在复发率等方面与外科手术治疗差距逐渐缩小,但其局限性较大,多瘘口及血管迂曲严重时,介入技术治疗效果较外科手术治疗效果差,所以微创血管内栓塞不如手术中断瘘管分流可靠 [3] [8]。术中显微镜和影像学的进步增强了我们手术治疗这些病变的能力 [9] [10]。
国外研究表明,部分SDAVF患者在术后出现原有症状加重,特别是括约肌功能障碍较术前明显(主观或客观上),对大多数人来说,这种症状加重的情况是短暂的,但是在极小部分患者术后随访中,运动或括约肌功能障碍的症状持续存在 [11] [12]。这种情况有可能是瘘口闭塞后血栓形成所致,术后抗凝治疗显得尤为重要 [9]。神经外科病患人群中,低分子肝素能有效预防静脉血栓栓塞,需要对这些患者采取更加个性化的治疗方法 [13]。抗凝治疗在术后1~2 d开始进行;此前主要口服华法林至少持续3个月,使凝血酶原活动度下降到正常的20%~50%。患者在术后3个月之后,如症状没有完全恢复,应该继续服用3~6个月 [14]。
NOTES
*第一作者。
#通讯作者。