摘要: 49岁男性,因“头痛3 d,左眼眼红眼痛2 d”入院(Vod0.8, Vos0.3, NCTod13.8 mmHg, os9.9 mmHg)。裂隙灯检查见左眼混合充血(++),角膜水肿(+),角膜后可见尘状沉着物(+++),前房积脓,液平高1 mm,瞳孔圆,d = 3 mm,对光反射迟钝,晶状体皮质不均匀灰白色混浊,眼底窥不清。右眼无特殊。初步诊断为急性虹膜睫状体炎。鉴别诊断为眼内炎。患者入院后,予以局部抗炎、局部及全身抗感染、玻璃体切除术治疗。术后随访视力恢复可。讨论:患者有疑似眼内炎的非特征性症状出现时,应考虑是否有内源性眼内炎的可能,一旦确诊立即对眼内炎症病灶做出相应治疗措施,挽救患者的视力,降低后遗症的发生率。
Abstract:
A 49-year-old man was admitted with headache for 3 days and red and pain for 2 days in the left eye. Visual acuity was 0.8 in the right eye and 0.3 in the left. The left eye was revealed under slit lamp to be with mixed hyperemia (++), corneal edema (+), KP (+++), anterior chamber empyema, fluid level 1mm, pupil circle, d = 3 mm, and the light reflection is slow, the lens cortex is uneven and grayish and cloudy, and the fundus is unclear. The right eye is nothing special. NCT: od13.8 mmHg, os9.9 mmHg. The initial diagnosis was acute iridocyclitis. The differential diagnosis is endophthalmitis. After the patient was admitted to the hospital, he was treated with local anti-inflammatory, local and systemic anti-infection, and vitrectomy. The visual acuity can be recovered after the follow-up. Discussion: When the patient has non-characteristic symptoms suspected of endophthalmitis, it should be considered whether there is the possibility of endogenous endophthalmitis. Once the diagnosis is made, corresponding treatment measures should be taken to the inflammatory lesions in the eye to save the patient’s vision and reduce the sequelae the rate of occurrence.
1. 前言
肺炎克雷伯杆菌导致的内源性眼内炎原发感染灶多见于肝脓肿,以肺部感染为原发感染灶的目前少有报道,视网膜下脓肿在内源性眼内炎的病例中极其少见。本病例报道一例原发感染灶为肺炎克雷伯杆菌性肺炎的内源性眼内炎,并且已经形成视网膜下脓肿,对于此种情况应及时行玻璃体切除手术并清除眼内病灶,以及时获得挽救患者视力机会。
2. 资料
2.1. 一般资料
患者男性,49岁。因“头痛3 d,左眼眼红眼痛2 d”来我院就诊。就诊3 d前出现双侧颞部持续性胀痛,2 d前出现眼红、眼痛,伴左眼视力下降。既往糖尿病史4年,血糖控制差。否认眼部手术史及外伤史。眼部检查:Vod0.8,Vos0.3,NCTod13.8 mmHg,os9.9 mmHg。眼混合充血(++),角膜水肿(+),角膜后可见尘状沉着物(+++),前房积脓,液平高1 mm,瞳孔圆,d = 3 mm,对光反射迟钝,晶状体皮质不均匀灰白色混浊,眼底窥不清(图1),右眼前后节未见明显异常。以左眼急性虹膜睫状体炎收入院。入院后左侧颞部疼痛加重,体温38.7℃,眼睑红肿,眼球内、外转方向受限。
2.2. 其他检查
餐后血糖 > 33.3 mmol/L,PH校正值7.29,血清β羟丁酸3.9 mmol/L,尿酮体10 mmol/L,白细胞计数16.46 × 109/L,嗜中性粒细胞百分比93.7%,糖化血红蛋白11.3%,血培养示肺炎克雷伯杆菌(+),真菌D-葡聚糖(−),房水未培养出真菌及细菌。胸部CT示双肺胸膜下多发感染性病灶(图2);眼部超声示左侧玻璃体内7~11点钟等回声团(图3);心脏彩超、肝胆胰脾超声等未见异常。

Figure 1. Photographs of the anterior segment of the patient’s eye on admission, empyema in the anterior chamber of the left eye, and ciliary hyperemia
图1. 入院时患眼前节段照相,左眼前房积脓,睫状充血

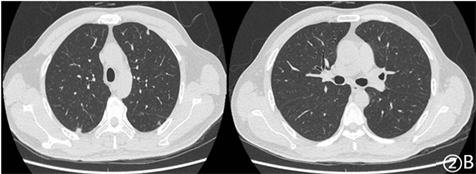
Figure 2. (A) CT of the chest shows multiple infectious lesions near the pleura; (B) CT of the chest shows obvious absorption of the original infectious lesions near the pleura
图2. (A) 胸CT可见近胸膜处多发的感染性病灶;(B) 胸CT可见近胸膜处原有的感染性病灶明显吸收
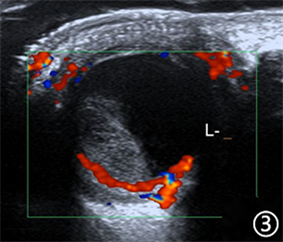
Figure 3. Color Doppler ultrasound shows the echo group at 7~11 o’clock in the left vitreous body
图3. 眼部彩超示左侧玻璃体内7~11点钟等回声团
更正诊断:左眼内源性眼内炎、左眼全眼球炎、肺炎克雷伯杆菌肺炎、肺炎克雷伯杆菌败血症、2型糖尿病并酮症酸中毒。经验性使用万古霉素 + 头孢他啶行左眼玻璃体腔注药治疗,据药敏试验结果予头孢哌酮舒巴坦 + 左氧氟沙星全身抗感染治疗。复查眼部彩超提示左侧玻璃体内液化成分较前增多(图4)。急行手术治疗,术中见玻璃体混浊,4~10点周边部视网膜巨大裂孔,网膜隆起,网膜下有大量黄白色粘稠脓液(图5)。术中取玻璃体液检测示:IL-6:13,045.2 pg/mL,革兰氏阴性菌脂多糖2.5 EU/mL,病毒及真菌均为阴性,提示革兰阴性菌感染。术后继续抗炎、抗感染治疗,术后3 d左眼矫正视力0.15,眼底照相示玻璃体腔硅油填充(图6),视盘界清,黄斑中心凹反射消失,视网膜平伏,可见少许渗出灶(图7)。术后2 w复查血培养结果阴性,血常规正常,胸部CT示病灶较前明显吸收(图2(B))。术后1月复查眼部B超示玻璃体腔内透声尚好,网膜未见明显异常,可见多条稍强回声光带。

Figure 4. Reexamination of eye color Doppler ultrasound after intravitreal injection treatment with vancomycin + ceftazidime showed that the left vitreous intravitreal echoes at 7~11 o’clock were similar in size, with more liquefied components
图4. 使用万古霉素 + 头孢他啶行左眼玻璃体腔注药治疗后复查眼部彩超示玻璃体左侧玻璃体内7~11点钟等回声团,大小较前相仿,液化成分增多
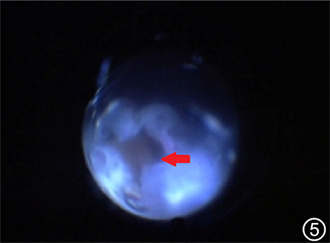
Figure 5. A subretinal abscess was found during the operation. There is a huge retinal hole with a size of about 2 PD. The retina around the hole is flocculent. The arrow indicates a yellow-white subretinal abscess
图5. 术中发现视网膜下脓肿。可见视网膜巨大裂孔,大小约2 PD,裂孔周围视网膜呈絮状,箭头所指黄白色即视网膜下脓肿

Figure 6. After the operation of the vitreous cavity B-ultrasound shows that the sound transmission in the vitreous cavity is still good, the omentum has no obvious abnormalities, and there are many slightly strong echo light bands (silicone oil)
图6. 术后玻璃体腔B超可见玻璃体腔内透声尚好,网膜未见明显异常,可见多条稍强回声光带(硅油)

Figure 7. Postoperative fundus photography showed the silicone oil filling state in the vitreous cavity of the left eye, the retina was flat and there were a few exudates. In the figure, the arrow points to the edge of the original abscess cavity, and the omentum is now flat
图7. 术后眼底照相见左眼玻璃体腔内硅油填充状态,视网膜平伏,有少许渗出灶。图中箭头所指原脓腔边缘,现网膜已平伏
3. 讨论
内源性细菌性眼内炎是细菌血行播散穿透血眼屏障致病,70%~75%的内源性细菌性眼内炎的致病菌为肺炎克雷伯杆菌(klebsiella pneumoniae, KP),视力预后差于其他眼内炎患者 [1] [2]。KP荚膜可以抵抗巨噬细胞的吞噬作用,除原发感染部位外,易发生其他器官迁移感染,最常见的原发感染灶是肝脓肿,故对于KP感染的眼内炎患者,需进行肝脓肿的排查,对眼内炎的诊治有指导和参考意义 [3] [4]。本病例排除其他系统的感染后,发现原发感染灶是较为少见的肺部感染。因此,对内源性眼内炎患者也要注意全身其他脏器的检查。糖尿病尤其是血糖控制不佳,引起中性粒细胞的趋化和吞噬作用减弱,这也是KP患者继发眼内炎的危险因素,如本文所报道病例。
肺炎克雷伯杆菌性眼内炎(endogenous klebsiella pneumoniae endophthalmitis, EKPE)早期可表现视力下降、眼红、眼痛、前房积脓等,易误诊为葡萄膜炎、结膜炎、闭角型青光眼等疾病 [5]。对于有上述症状应排除是否有眼底的病变,眼底不能窥入的病人需要及时进行B超检查。本例患者最初表现为头痛、眼痛和前房积脓,与前葡萄膜炎症状十分相似,要注意鉴别,避免误诊。
KP细菌毒素对眼部组织破坏力大,强烈炎症反应可在24H内损伤视网膜功能 [4] [6]。抗生素药物很难经过血房水屏障和血视网膜屏障到房水和玻璃体中,全身应用抗生素效果欠佳。当感染致病性强的细菌、并发玻璃体混浊或视网膜脱离时,及早行玻璃体切除术,减少眼内细菌和炎性负荷,帮助抗生素渗透到视网膜下感染灶,同时加强全身抗感染治疗,增加挽救眼球和改善视力的机会 [7] [8]。本患者入院后眼部症状加重,视力进行性下降,出现眼外肌麻痹症状,经验性使用广谱抗生素行玻璃体腔注药治疗,症状无明显好转。根据患者血培养及药敏试验结果选用敏感抗生素抗感染治疗,同时行玻璃体切除术。术中发现视网膜下脓肿,这在内源性眼内炎病例中少见,仅占5% [9],由于感染的范围及程度的不同,视网膜下脓肿的治疗无统一方法,目前文献报道的方法有静脉注射抗生素、玻璃体内注射抗生素、玻璃体切除、视网膜切除、对脓肿进行切开引流、以及视网膜下脓肿穿刺引流等。Tsai TH和Peng KL认为视网膜下脓肿小于4 PD,玻璃体腔内注射抗生素同时进行玻璃体切除可以避免进行视网膜切开 [10]。Venkatesh等人曾在玻璃体切除后直接将万古霉素注射到脓腔中,术后脓肿迅速吸收 [11]。Xu H等人报道过仅进行玻璃体切除而未进行视网膜切开术和脓肿抽吸术的案例 [12]。本例中视网膜大片坏死脱离,下方可见大量的黄白色脓苔,在进行玻璃体切除后,彻底清除视网膜下脓肿及坏死组织,防止感染进一步扩大加重,对脓腔周边的视网膜进行激光光凝,玻璃体腔内填充硅油。术后患者眼部症状明显好转,视力部分恢复,网膜平伏。
4. 总结
在临床工作中,对高龄、糖尿病患者或有免疫抑制或缺陷的患者,当出现视力下降、眼红、眼痛、前房积脓等非特异性的症状或体征时,应考虑是否有内源性眼内炎的可能,尤其是眼底无法窥清时,及时进行眼部B超等检查排除眼内炎,积极寻找病因,全面检查眼部情况,及时排除眼内炎。一旦确诊立即对眼内炎症病灶做出相应治疗措施,挽救患者的视力,降低后遗症的发生率。
注:本篇病例报告已获得病人知情同意。
NOTES
*通讯作者。