摘要: 目的:分析嗜酸粒细胞性胃肠炎(eosinophilic gastroenteritis, EG)临床特征,为诊断和治疗提供思路。方法:本研究通过对本院诊断的1例嗜酸粒细胞胃肠炎浆膜型病例行回顾分析并随访,患者男,39岁,因“腹胀伴腹泻2周”入院。行全腹CT示腹腔积液,血常规示嗜酸粒细胞计数7.47 × 10
9/L。胃镜病理:胃和十二指肠球部每高倍镜视野内嗜酸粒细胞个数3~14个。腹水病理:镜下见较多量嗜酸粒细胞及少量中性粒细胞。予大剂量激素冲击及小剂量维持治疗。结果:患者经治疗后随访未再出现复发。结论:嗜酸粒细胞性胃肠炎是一种少见的嗜酸粒细胞(eosinophilic granulocyte, EoS)增多的胃肠疾病,其侵及浆膜层时可表现为大量嗜酸性腹水,其临床表现多样,患者多伴随过敏史,糖皮质激素治疗有效。
Abstract:
Objective: To analyze the clinical characteristics of eosinophilic gastroenteritis and provide ideas for diagnosis and treatment. Methods: In this study, a case of serosal eosinophilic gastroenteritis diagnosed in our hospital was retrospectively analyzed and followed up. The patient was 39 years old and was admitted to the hospital with “abdominal distension and diarrhea for 2 weeks”. A CT scan of the whole abdomen showed fluid in the abdominal cavity, and a routine blood test showed an eosinophil count of 7.47 × 109/L. Gastroscopy pathology: The number of eosinophils per high-power field of the stomach and duodenal bulb is 3~14. Ascites pathology: More eosinophils and a few neutrophils were seen under the microscope. Give high-dose hormone shock and low-dose maintenance treatment. Results: The patient did not relapse after follow-up after treatment. Conclusion: Eosinophilic gastroenteritis (eosinophilic gastroenteritis, EG) is a rare gastrointestinal disease with increased eosinophilic granulocyte (EoS), which can manifest as a large amount of eosinophilia when it invades the serosal layer. Its clinical manifestations are diverse, most patients are accompanied by a history of allergies, and glucocorticoid therapy is effective.
1. 引言
嗜酸粒细胞性胃肠炎(Eosinophilic gastroenteritis, EG)是一种少见的嗜酸粒细胞(Eosinophilic granulocyte, EoS)增多的胃肠疾病,随着医疗技术的进展,近年来发病率逐渐升高。其诊断主要依靠临床表现、实验室检查、影像学检查、内镜及组织病理学结果,虽有证据显示内镜下表现无特异性 [1],但组织病理学结果始终作为诊断EG的金标准。
2. 病例资料
患者男,39岁,因“腹胀伴腹泻2周”入院。既往过敏性鼻炎、支气管哮喘病史,父母均有过敏病史。该患者入院2周前无明显原因出现腹胀,伴腹泻,2~3次/天,为黄色稀水样便,无发热。行全腹CT示腹腔积液,右下腹腔部分小肠轻度扩张积气、肠壁水肿样改变(如图1、图2所示)。以“腹腔积液”收入院。查体:全身皮肤未见皮疹,腹部膨隆、对称,移动性浊音阳性。辅助检查:血常规示嗜酸粒细胞计数7.47 × 109/L;嗜酸粒细胞百分率55.30% (参考范围:嗜酸粒细胞0.02~0.52 × 109/L,嗜酸粒细胞百分率0.4%~8.0%)。胃镜检查示慢性非萎缩性胃炎伴糜烂,十二指肠炎症(如图3所示)。病理:慢性非萎缩性胃炎,中度炎症;少许小肠粘膜呈中度慢性炎;胃和十二指肠球部每高倍镜视野内嗜酸粒细胞个数3~14个(如图4所示)。腹水病理:镜下见较多量嗜酸粒细胞及少量中性粒细胞。食物不耐受筛查14项示牛奶、蛋白/蛋黄、小麦阳性。粪便常规:阴性,未见虫卵。余免疫球蛋白测定、抗核抗体、抗中性粒细胞胞浆抗体、风湿四项、T-SPOT、ESR、多种肿瘤标志物、肝肾功均未见明显异常。诊断为嗜酸粒细胞性胃肠炎。予甲强龙80 mg静脉滴注冲击治疗。3天后复查血常规示嗜酸粒细胞恢复正常,患者腹胀症状减轻,腹围下降。甲泼尼龙(美卓乐) 40 mg口服并逐渐减量维持治疗,同时嘱患者避免食用过敏食物。患者出院后3月复查血常规无异常,后因嗜酸粒细胞升高1月再次入院。进一步完善骨髓穿刺示有核细胞增生活跃,嗜酸粒细胞占比19%。骨髓染色体核型分析、融合基因-FIP1L1/PDGFRA、融合基因-TEL/PDGFRB未见异常。出院后继续予甲泼尼龙(美卓乐) 20 mg口服维持治疗并逐渐减量,随访观察半年,至本文总结前(2021-4-30)患者无外周血嗜酸粒细胞升高及腹痛、腹泻、腹胀等不适,复查超声未再探及腹水。采集并使用患者信息已获得患者本人知情同意。
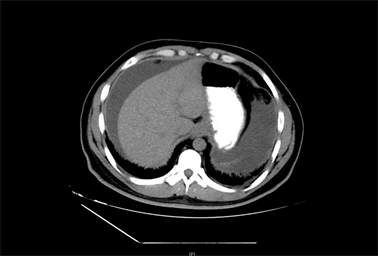
Figure 1. A large number of water-like density shadows are seen in the abdominal cavity
图1. 腹腔内见大量水样密度影
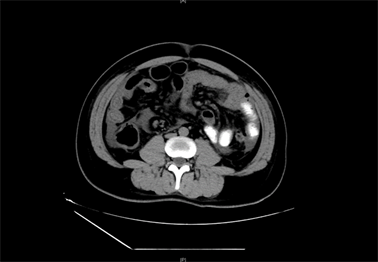
Figure 2. Part of the small intestinal wall of the right lower abdominal cavity edema-like changes
图2. 右下腹腔部分小肠壁水肿样改变

Figure 3. Deformation of the duodenal bulb, mucosal congestion, edema, and flaky redness can be seen in the anterior wall of the bulb and the initial segment of the descending part
图3. 十二指肠球部变形,球部前壁及降部起始段可见粘膜充血水肿、片状发红

Figure 4. A large number of eosinophils are seen in the duodenal mucosa as marked in the picture, HE staining 400× field of view
图4. 十二指肠黏膜见大量嗜酸性粒细胞,如图标志,此图为HE染色400×视野
3. 讨论
嗜酸粒细胞胃肠病(Eosinophilic gastrointestinal disorders, EGID)是一种病因不明且相对罕见的胃肠道炎症性疾病,包括嗜酸粒细胞性食管炎(Eosinophilic esophagitis, EoE)、嗜酸粒细胞性胃肠炎(EG)、嗜酸粒细胞性结肠炎(Eosinophilic colitis, EoC)。调查发现在日本EG的男女比例为1.2:1,男性占优势,在美国则为女性占优势 [2]。据报道,45%至63%的EG病例会伴有过敏性疾病,包括哮喘、鼻炎、湿疹和药物或食物不耐受症 [3],故认为EG病因可能与过敏及IgE介导的TH2变态反应相关 [4] [5]。EG患者通常有外周血嗜酸粒细胞计数的升高,但约1/3的患者无外周血嗜酸粒细胞升高。临床表现常与病变浸润的范围及深度有关,黏膜层病变患者常表现为恶心、呕吐、腹痛、腹泻和腹部膨隆等,肌层病变患者常出现完全或不完全梗阻症状,浸润浆膜层的患者则表现为腹腔积液,存在弥漫性小肠病变或肠炎的患者可发生营养吸收不良、蛋白丢失性肠病、缺铁性贫血和体重减轻 [1]。目前,EG发生率约8.4~28/100,000 [3],以腹水为首发症状报告病例在国内外均较罕见。内镜及组织病理学诊断非常重要,内镜下表现常不具有特异性,除胃黏膜呈结节状或息肉状、胃壁增厚、黏膜糜烂,重度病例还可出现深部溃疡,看似正常的黏膜同样存在嗜酸粒细胞聚集,故应从胃肠道取至少5~6个活检样本(包括肉眼可见正常及异常部位) [1],如果只对异常部位进行活检,则有较高的漏诊率。因此建议对疑诊为EG患者行胃镜、结肠镜和小肠镜进一步明确诊断。本例患者因腹泻、腹痛等不适症状及CT提示肠壁水肿未行小肠镜及结肠镜。
至今为止EG的诊断标准尚不明确,目前通用的Talley标准为:① 胃肠道症状,② 病理学及体液检查提示嗜酸粒细胞浸润(嗜酸粒细胞增高 > 20每高倍视野具有重大意义),③ 无胃肠道以外多器官嗜酸粒细胞浸润,④ 排除其他引起嗜酸粒细胞浸润的疾病,如寄生虫感染、过敏反应、淋巴瘤、炎症性肠病等 [6]。除此之外,其鉴别诊断应包括嗜酸细胞增多综合征(Hypereosinophilic syndrome, HES)。HES是指长期组织中嗜酸细胞升高引起的全身性疾病,首发症状部分与EG相似,还可以累及皮肤、肺部、心脏、肝脾、神经系统、血液系统等,严重者可出现心肌内膜纤维化、限制性心肌肥大、心脏瓣膜瘢痕导致瓣膜回流及附壁血栓形成。其发病率为0.036/100,000,死亡率9.3% [7],预后较单纯EG差。当患者长期嗜酸粒细胞升高,需警惕发生慢性嗜酸粒细胞性白血病的可能,本例患者通过完善骨髓穿刺及相关基因分型,进一步排除了此类血液系统疾病。
有研究认为,EG是一种自限性疾病,约42%的患者可自行缓解 [8]。经验性饮食治疗可缓解46%患者 [9]。在临床治疗中,糖皮质激素能够抗炎、抗过敏、降低嗜酸粒细胞趋化,对于复发型的EG,激素治疗起始量应足,适当延长用药时间可减少复发率。一项关于88例诊断为EG患者的回顾性研究发现,全身应用糖皮质激素治疗快速、有效,但有1例患者长期激素治疗后出现感染性休克并发症 [10]。考虑长期应用激素的不良反应,对于症状较轻的患者,可给予肥大细胞膜稳定剂(如酮替芬)、免疫抑制剂(如硫唑嘌呤)或白三烯受体拮抗剂(如孟鲁司特钠)治疗,但有研究认为除激素外的用药均未实现临床缓解 [11]。各种类型的靶向治疗研究正在进展中 [12]。
综合本例,不明原因腹水伴外周血嗜酸粒细胞升高的患者应排除嗜酸细胞性胃肠炎可能。本病患者常伴有家族性过敏史,食物过敏可能为发病原因之一。通过胃镜、腹水穿刺等相关检查可获得诊断必要证据,尤其应注意内镜下多点活检。诊断时还需鉴别引起嗜酸粒细胞升高的其他疾病,特别是嗜酸粒细胞增多综合征要引起临床高度重视。EG具有自限性特点,糖皮质激素治疗有效,但停药过早有较高的复发率,注意加强患者教育及随访。