摘要: 目的:探讨利用磁共振q-Dixon技术鉴别脊柱血管瘤和脊柱常见恶性肿瘤的价值。材料和方法:收集自2021年1月至2021年8月经病理证实或经长期随访证实的脊柱血管瘤和脊柱常见恶性肿瘤各30例。所有患者均行常规MRI检查及q-Dixon检查,扫描数据上传至Siemens syngo.via工作站,经后处理获得FF图(脂肪分数图)。在FF图上勾画感兴趣区(Region of interest, ROI)得到FF值,对符合正态分布的数据以平均值 ± 标准差表示,使用独立样本t检验分析两组间脂肪含量差异的统计学意义。利用受试者工作特性曲线(Receiver operating characteristic curve, ROC曲线)分析其诊断效能。结果:脊柱恶性肿瘤FF值为(11.55 ± 7.31)%,脊柱血管瘤FF值为(58.6 ± 15.70)%。脊柱恶性肿瘤的FF值小于血管瘤的FF值,两组数值间的差异具有统计学意义(t = 14.90, P < 0.001),绘制FF值对脊柱血管瘤和脊柱常见恶性肿瘤鉴别诊断效能的ROC曲线,AUC为1.00,敏感度和特异度为100%,鉴别脊柱血管瘤和恶性肿瘤的FF值的临界值为25.0%。结论:磁共振q-Dixon技术对鉴别脊柱血管瘤和脊柱常见恶性肿瘤具有良好的诊断价值。
Abstract:
Purpose: To evaluate the value of q-Dixon technique in distinguishing spinal hemangioma from spinal malignancy. Materials and methods: A total of 30 cases of spinal hemangioma and common malignant tumors of the spine proved by pathology or clinical follow up were collected from January 2021 to August 2021. All patients underwent conventional MRI and q-Dixon examination. The scan data were uploaded to Siemens syngo.via workstation and FF map (fat fraction map) was obtained after post-processing. The region of interest (ROI) was delineated on the FF map to obtain FF values, and the data with normal distribution were expressed as mean ± standard deviation. The inde-pendent sample T test was used to analyze the statistical significance of fat content differences be-tween the two groups. Receiver operating characteristic curve (ROC curve) was used to analyze its diagnostic efficiency. Results: The FF value of spinal malignant tumor was (11.55 ± 7.31)% and that of spinal hemangioma was (58.6 ± 15.70)%. The FF value of spinal malignancies was smaller than that of hemangiomas, and the difference between the two groups was statistically significant (t = 14.90, P < 0.001), the ROC curve of FF value for differential diagnosis of spinal hemangioma and common spinal malignant tumor was drawn. The area under the curve (AUC) was 1.00, the sensitiv-ity and specificity were 100%, and the critical value for differential diagnosis of spinal hemangioma and malignant tumor was 25.0%. Conclusion: MRI q-Dixon technique has good diagnostic value in distinguishing spinal hemangioma from common spinal malignancies.
1. 引言
脊柱血管瘤是常见的椎体良性肿瘤,大多因含有明显的脂肪成分和MRI典型征象很容易诊断。但也可以有非典型和侵袭性表现,Gaudino [1] 等人将血管瘤分为3种类型:典型、非典型和侵袭性。“典型”和“非典型”主要指的是磁共振表现,它与组织病理学特征(脂肪与血管成分的比率以及间质水肿)直接相关。脂肪含量较多时(典型表现),T1WI及T2WI均成高信号,压脂像成稍低信号影。血管成分含量较多时(非典型表现),T1WI成低或稍高信号影,T2WI及压脂像成高信号影。侵袭性指的是脊柱血管瘤侵袭性生长,并造成椎体、椎板或椎弓根的膨胀性改变、或形成椎旁软组织肿块 [2],侵袭性血管瘤通常都具有非典型的影像表现。这些非典型和侵袭性血管瘤与脊柱原发性恶性肿瘤或转移瘤表现相似,有时难以区别。对于脊柱恶性肿瘤 [1] 的MRI信号改变大多是由于病灶取代正常的脂肪骨髓,降低脊柱脂肪含量导致。通过以上分析可知,脊柱血管瘤与脊柱恶性肿瘤可以有相似的影像学表现,但脂肪含量不同,因此可通过测定脂肪含量来鉴别二者。
临床实践中,许多研究已探索了对骨髓脂肪进行量化的方法。Dixon [3] 在1984年提出,利用水和脂肪中质子进动频率不同,分别采集水和脂肪相位差为0˚ (即同相位)和相位差为180˚ (即反相位)图像,即Dixon两点法。但因Dixon两点法对磁场B0不均匀敏感及扫描时间长等原因,影响图像质量,限制了它在临床中的应用。Glover [4] 和Schneider [5] 在1991年提出Dixon三点法,通过增加第三组图像来补偿对磁场B0不均匀敏感,避免了相位误差,增加了组织对比的效果。这些改良后的Dixon三点法包括q-Dixon (Siemens Healthcare)、m-Dixon (Philips Healthcare)和IdealIQ (GE Healthcare)。本文研究目的是应用q-Dixon技术,即一次扫描得到4幅定量图像即水含量图、脂肪含量图、T2*图和R2*图,并经后处理自动生成FF图(脂肪分数图),定量脊柱血管瘤和脊柱常见恶性肿瘤病灶中的脂肪含量。探讨通过脂肪含量的差异鉴别脊柱血管瘤和脊柱常见恶性肿瘤的可行性和价值。
2. 资料和方法
2.1. 研究对象
自2021年1月至2021年8月连续纳入63名患者,所有患者均签署知情同意书。纳入标准:1) 肿瘤发生在脊柱。2) 诊断经病理学证实的脊柱恶性肿瘤和血管瘤患者。3) 诊断经长期随访病灶大小未见明显变化、未出现相应症状而证实的脊柱血管瘤患者。4) 均行常规MRI检查和q-Dixon检查。排除标准:1) MRI检查禁忌症及不能配合检查者。2) 病灶太小,无法在FF图上显示局部骨病变的感兴趣区(ROI)。3) 发生在椎管或椎旁软组织的病灶。另外3名患者的FF图在图像分析过程出现了计算错误,可能因为外界因素干扰磁场导致磁场不均匀,也被排除于研究之外。因此我们的研究包括经病理学或随访证实确诊的60名患者。脊柱血管瘤30例(男7例,女23例,年龄范围26~77岁,平均年龄约59岁)。脊柱常见恶性肿瘤30例(男21例,女9例,年龄范围42~82岁,平均年龄约61岁)。脊柱血管瘤中有2例侵袭性血管瘤。脊柱恶性肿瘤包括转移瘤(11例)、多发性骨髓瘤(18例)、非霍奇金淋巴瘤(1例)。
2.2. 仪器与方法
采用美国Siemens3.0TMRI扫描仪,取仰卧位,体部阵列线圈,头先进。行常规MRI扫描(矢状位T1WI水抑制、T2WI、压脂T2WI和横断位T2WI)和q-Dixon (横断位、矢状位)扫描。扫描参数见表1。

Table 1. MRI scan sequence parameters
表1. 磁共振扫描序列参数
2.3. 图像分析
q-Dixon序列扫描后通过Siemens syngo.via工作站后处理得到FF图,由2名肌骨组的影像诊断专家按照ROI勾画标准并在横断位/矢状位FF图上进行ROI勾画测量FF值,ROI勾画标准:ROI面积大于0.50 cm2,最大范围的包括整个病灶,尽量避开骨皮质、椎基静脉等,取两位医师测量值的平均值,分别得到脊柱血管瘤和脊柱常见恶性肿瘤的FF值。
2.4. 统计方法
采用SPSS24.0软件及Medcalc软件对数据进行统计分析,利用SPSS24.0软件检测两组数据均符合正态分布,以平均值 ± 标准差表示,并采用独立样本t检验分析两组数据间脂肪含量的统计学意义,以P < 0.05为差异有统计学意义。利用Medcalc软件绘制受试者工作特性曲线(ROC曲线),计算曲线下面积(AUC值)、敏感度、特异度及临界值。
3. 结果
脊柱恶性肿瘤病灶脂肪含量(11.55 ± 7.31)%,脊柱血管瘤病灶脂肪含量(58.6 ± 15.70)%。采用独立样本t检验得出脊柱血管瘤与脊柱恶性肿瘤脂肪含量差异具有统计学意义(P = 0 < 0.001)。脊柱恶性肿瘤脂肪含量低于脊柱血管瘤(见图1、图2)。绘制脊柱血管瘤与常见恶性肿瘤脂肪含量的ROC曲线(见图3),AUC值为1.00,敏感度和特异度为100%,临界值为25% (见表2)。说明q-Dixon序列对鉴别脊柱血管瘤与脊柱恶性肿瘤具有很好的诊断效能。
 (A)
(A)  (B)
(B)
Figure 1. A 60-year-old woman with multiple metastases to the spine. A: Sagittal T1WI showed diffuse decreased signals in L4 and T11 vertebral bodies. B: The cross-sectional FF diagram of q-Dixon sequence automatic reconstruction shows that FF value is 5.7%
图1. 女,60岁,脊柱多发转移瘤。A:矢状位T1WI显示L4、T11椎体信号弥漫性减低。B:q-Dixon序列自动重建横断位FF图显示FF值为5.7%
 (A)
(A)  (B)
(B)
Figure 2. A 41-year-old woman with L3 vertebral hemangioma. A: The sagittal view of T1WI showed nodular hypersignal shadow of L3 vertebral body with clear boundary. B: The cross-sectional FF diagram of q-Dixon sequence automatic reconstruction shows the FF value of 64.56%
图2. 女,41岁,L3椎体血管瘤。A:T1WI压脂矢状位显示,L3椎体结节状高信号影,边界清。B:q-Dixon序列自动重建横断位FF图显示FF值64.56%
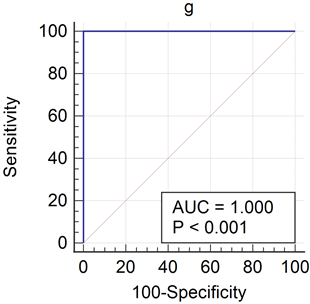
Figure 3. ROC curve of fat content in spinal hemangioma and common malignancies
图3. 脊柱血管瘤与常见恶性肿瘤脂肪含量的ROC曲线

Table 2. Diagnostic performance of FF value in distinguishing spinal hemangioma from common spinal malignancies
表2. FF值鉴别脊柱血管瘤与脊柱常见恶性肿瘤的诊断性能
4. 讨论
大多数脊柱血管瘤因含有脂肪成分及典型的MRI表现,如横断位圆点征,矢状位栅栏征等较容易鉴别 [6],但也可以有非典型和侵袭性表现,Gaudino等人将血管瘤分为3种类型:典型、非典型和侵袭性。“典型”和“非典型”主要指的是磁共振表现,它与组织病理学特征(脂肪与血管成分的比率以及间质水肿)直接相关。脂肪含量较多时(典型表现),T1WI及T2WI均成高信号,压脂像成稍低信号影。血管成分含量较多时(非典型表现),T1WI成低或稍高信号影,T2WI及压脂像成高信号影。侵袭性指的是脊柱血管瘤侵袭性生长,并造成椎体、椎板或椎弓根的膨胀性改变、或形成椎旁软组织肿块 [2],侵袭性血管瘤通常都具有非典型的影像表现。这些非典型和侵袭性血管瘤与脊柱原发性恶性肿瘤或转移瘤表现相似,有时难以区别。本文研究中所选取的所有脊柱血管瘤病例均为非典型和侵袭性血管瘤,与脊柱恶性肿瘤的影像表现有一定的重叠。传统方法中,多采用常规MRI序列定性评估脊柱信号改变,通过肉眼观察脊椎信号在T1WI、T2WI及压脂像的变化及比较脊椎信号与邻近椎间盘信号的差异来评估病变性质,虽敏感度较高,但特异性低 [7] [8]。因此,许多研究探索了对骨髓脂肪进行量化的方法,之前有文献报道通过同反相位化学位移编码成像定量骨髓脂肪含量来鉴别脊柱良恶性病变,结果表明,反相位信号强度比同相位信号强度下降20%作为鉴别脊柱良恶性病变的临界值 [7] [9]。但同反相位化学位移编码成像在定量脂肪含量时存在许多混杂因素,包括主磁场不均匀性效应、脂肪谱中多峰的存在、T2*效应、T1*效应、涡流效应等,使脂肪定量不准确 [9] [10]。
MRS (单体素磁共振波普)是精确量化椎体局部脂肪含量的金标准,但由于操作复杂,耗时长,易受低空间分辨率相关的采样误差的影响,临床实践中多不采用 [11]。随着MRI技术的进步,改良的Dixon技术越来越多的运用于椎体脂肪定量分析中。从Dixon二点法到Dixon三点法,许多混杂因素都被最小化,包括T2*衰减、T1偏移、B0磁场不均匀性、脂肪频谱复杂性、噪声偏移和涡流效应等 [12]。它可用于不同的临床MRI系统,包括q-Dixon (Siemens Healthcare)、m-Dixon (Philips Healthcare)和IdealIQ (GE Healthcare)。Dixon三点法相较于MRS更易操作,采集时间短,可重复性良好 [13],且通过自动生成的FF图可直接测量脂肪分数。且已有文献报道指出,利用Dixon技术测量脂肪含量与MRS定量脂肪有很好的一致性。本文利用磁共振q-Dixon (Siemens Healthcare)技术,经后处理自动生成FF图,定量脊柱血管瘤和脊柱常见恶性肿瘤病灶中的脂肪含量,研究结果表明,FF值对鉴别脊柱血管瘤与脊柱常见恶性肿瘤具有较高的诊断性能(AUC值为1.00,敏感度和特异度为100%),临界值为25%。
之前有文献报道过利用改良的Dixon技术鉴别脊柱良恶性病变,如Kim [14] 等人利用三维容积梯度回波序列,通过T2*校正的FF图鉴别恶性骨髓替代病变和良性红骨髓沉积的可行性。研究结果表明FF图可以用来区分良恶性病变(AUC = 0.961,敏感度85.7%,特异度100%),与我们的研究结果相似(AUC = 1.00,敏感度100%,特异度100%)。但我们的诊断性能更高,可能因为之前研究的良性改变是红骨髓沉积,而且主要是高细胞性红骨髓沉积,造血细胞丰富,T1WI成低信号。而本文研究的良性肿瘤是血管瘤,脂肪含量较多,FF值较大,与脊柱恶性肿瘤FF值间相差更大,诊断性能更高。
我们的研究也有局限性,首先,我们的样本数量较少,没有专门收集到足够多的侵袭性血管瘤样本数与脊椎恶性肿瘤单独进行比较。第二,我们没有将q-Dixon技术与其他技术进行比较。
5. 结论
磁共振Dixon序列能够精确定量出脊椎血管瘤和脊椎常见恶性肿瘤骨髓脂肪含量的差异,脊椎血管瘤的脂肪含量大于常见恶性肿瘤的脂肪含量,磁共振q-Dixon技术对鉴别脊柱血管瘤和脊柱常见恶性肿瘤具有良好的诊断价值。
基金项目
国家自然科学基金资助项目(81571673)。
NOTES
*通讯作者Email: zrz19830426@qdu.edu.cn