摘要: 目的:探讨应用超声心动图左心房径线指数(LADi)评价心房颤动患者心脏射频消融术后短期复发的价值。方法:回顾性分析自2018年以来于我院诊断为心房颤动并首次接受心脏射频消融术患者242例,根据随访3~12个月内是否复发心房颤动,将其分为复发组(33例)和非复发组(209例),分析两组患者的一般临床资料,行超声心动图检查收集左心房前后径(D1)、左心房左右径(D2)、左心房上下径(D3),并计算径线平均值D,以体表面积标化D即为左心房径线指数(LADi),采用logistic回归方程分析心房颤动复发的相关因素,并使用受试者工作特征(ROC)曲线评价左心房径线指数预测心房颤动复发的价值。结果:复发组LADi明显高于未复发组,且差异有统计学意义(P < 0.05),回归分析显示,LADi为房颤短期复发的独立危险因素(OR = 1.251, 95% CI: 1.0931.431, P = 0.001),ROC曲线分析显示,LADi预测RFCA后房颤复发的曲线下面积为0.675 (95% CI: 0.5790.771, P = 0.01),LADi取截断值为27.54时,其敏感度为0.606,特异度0.695。结论:超声心动图左心房径线指数与RFCA术后房颤复发密切相关,有望成为临床预测RFCA术后房颤复发的新参数。
Abstract:
Objective: To investigate the value of ultrasonography left atrial radius index (LADi) to evaluate short-term recurrence of cardiac radiofrequency ablation in patients with atrial fibrillation. Meth-ods: Retrospectively analyze 242 patients diagnosed with atrial fibrillation in our hospital since 2018 and undergoing radiofrequency ablation for the first time; patients were divided into recur-rent atrial fibrillation groups (33 cases) and non-relapsing groups (209 cases) according to whether they recurred atrial fibrillation within 3~12 months of follow-up; analyze the general clinical data of the two groups, perform echocardiography to collect the anteroposterior diameter of the left atrium (D1), left and right diameter of the left atrium (D2), upper and lower diameter of the left atrium (D3), and calculate the average radius D. The left atrial radius index (LADi) was standardized by body surface area, the logistic regression equation was used to analyze the relevant factors of atrial fibrillation recurrence, and the subject’s working characteristics (ROC) curve was used to evaluate the value of the left atrial radius index to predict the recurrence of atrial fibrillation. Results: The LADi of the relapse group was significantly higher than that of the non-relapse group, and the dif-ference was statistically significant (P < 0.05), and regression analysis showed that LADi was an in-dependent risk factor for short-term recurrence of atrial fibrillation (OR = 1.251, 95% CI: 1.0931.431, P = 0.001), and the ROC curve analysis showed that the area under the curve of LADi predicting atrial fibrillation recurrence after RFCA was 0.675 (95% CI: 0.5790.771, P = 0.01). When the cut-off value of LADi was 27.54, its sensitivity was 0.606 and its specificity was 0.695. Conclusion: The left atrial radius index of echocardiography was closely related to the recurrence of atrial fibrillation after RFCA, and was expected to become a new parameter for clinical prediction of recurrence of atrial fibrillation after RFCA.
1. 引言
心房颤动(atrial fibrillation, AF)是一种好发于老年人群的心律失常,有研究表明在80岁以上老年人群中AF发生率大约为5%~15% [1]。AF可引起各种血栓栓塞疾病,比如脑动脉栓塞引起的脑梗死,大大降低患者的生活质量,严重者可危及生命 [2]。目前经导管射频消融术(radiofrequency catheter ablation RFCA)是临床上治疗AF的有效方法,但术后复发率可高达30% [3]。因此,找到一种便捷、准确的方法尽早识别术后复发的高危患者尤为重要。有研究 [4] 表明房颤射频消融术后复发与左心房大小有关。超声心动图是目前评估左心房大小的主要技术方法,其中应用改良双平面Simpson法定量左心房容积(left atrial volume, LAV)为评价左心房大小的推荐方法 [5]。但其因操作繁琐较难应用于临床,有研究 [6] 发现左心房径线指数(left atrial dimensional index, LADi)综合了左心房三个径线的大小,同时消除了体表面积的影响,且其操作简便、快捷,可作为评价左心房大小的参数。本研究旨在探讨LADi与AF术后复发之间的关系及其预测价值。本研究回顾性分析青岛大学附属医院(以下简称我院)行射频消融术的AF患者,探讨术前左心房径线指数对患者术后复发的预测价值,为术后复发高风险患者的治疗提供指导。
2. 对象与方法
2.1. 对象
本研究为回顾性研究,连续纳入2018年1月~2021年4月在我院住院行射频消融术的房颤患者242例。按照RFCA术后3~12个月之内房颤是否复发分为复发组(33例)和非复发组(209例)。房颤复发评价标准为接受消融术后按常规术后治疗方案接受利伐沙班、β受体阻滞剂、胺碘酮等药物治疗,并且3~12个月内复查心电图或行24 h动态心电图发现房颤。纳入标准:1) 首次行射频消融治疗;2) 有2016年ESC指南推荐的RFCA适应症。排除标准:1) 合并严重心脏瓣膜病;2) 合并严重肝肾功能不全;3) 患者有严重疾病,并发肿瘤、感染或免疫系统疾病,预期寿命不到1年;4) 随访失联。所有患者治疗前均签署知情同意书,并获取我院伦理委员会审批。
2.2. 方法
2.2.1. 资料收集
患者的一般资料通过查阅电子病历获取,包括性别、年龄、吸烟史、饮酒史、既往病史(充血性心力衰竭、高血压、糖尿病、脑卒中或短暂性脑缺血发作)等。患者的用药情况,包括抗凝药、控制心室率等药物通过由电子病历及门诊随访获取。
2.2.2. 超声心动图检查
采用Philips彩色多普勒超声诊断仪,S5-1矩阵探头,频率为1-5MHz。超声心动图图像采集:被检者取左侧卧位,平静呼吸,连接同步心电图,调整采集图像为三个心动周期,分别采集标准胸骨左缘左室长轴观和心尖四腔心观。左心房径线测量:于胸骨左缘左室长轴观,自大动脉根部后壁后缘垂直测量至左心房后壁前缘,测量左心房前后径(D1) (图1(B)),于心尖四腔心观,自房间隔中部至左心房侧壁,测量左心房左右径(D2),自二尖瓣环中点至左心房顶部,测量左心房上下径线(D3) (图1(A))。取D1、D2、D3的平均值记为D,以体表面积标化分别得到D1i、D2i、D3i、LADi [6]。
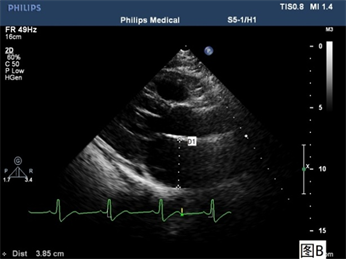
Figure 1. (A): Apical four chamber view; (B): Long axis of left ventricle view (D1: Anteroposterior diameter of the left atrium; D2: Left and right diameter of the left atrium; D3: Upper and lower diameter of the left atrium)
图1. (A):心尖四腔心观;(B):左室长轴观(D1:左心房前后径;D2:左心房左右径;D3:左心房上下径)
2.2.3. 电生理检查和导管射频消融
患者取平卧位,消毒双侧锁骨上下区及双侧腹股沟区皮肤,穿刺单侧锁骨下静脉,置6F鞘,沿鞘送冠状窦电极至冠状窦内。穿刺单侧股静脉,送8.5F swartz鞘至上腔静脉,沿鞘送房间隔穿刺针至卵圆窝,穿刺房间隔,将swartz送至左心房,沿鞘送Pentaray电极至左心房,在carto系统指导下建立左房模型,分别行双侧肺静脉前庭电隔离。患者若为持续性房颤,加做左房顶部线、底部线、前壁线、二尖瓣峡部线及三尖瓣峡部线的线性消融,若不能转复为窦性心律,则行体外电复律,观察30分钟,送Pentaray电极至右上肺静脉、右下肺静脉、左上肺静脉、左下肺静脉及各消融线均达到双向电隔离。每次射频应用持续30~50秒,温度保持在42℃,功率保持在30 W。术后据患者情况选用华法林或利伐沙班至少抗凝4周。
2.3. 随访
所有患者射频消融术后第3、6和12个月行心电图检查,期间如有不适则随时行心电图检查。随访期间根据需要进行24 h动态心电图监测。将房颤复发定义为消融3个月后常规心电图或动态心电图上记录的房颤、心房扑动或房性心动过速持续时间 ≥ 30 s [7]。
2.4. 统计学处理
采用SPSS 26.0软件进行统计学分析,正态分布的连续变量以
表示,组间比较使用两独立样本t检验;计数资料以百分构成比表示,组间比较采用x2检验;采用Logistic回归分析房颤复发的相关因素,采用受试者工作特征(receiver operating characteristic, ROC)曲线评估左心房径线指数对房颤复发的预测价值。P < 0.05为差异有统计学意义。
3. 结果
3.1. 临床基线资料
本研究共纳入首次接受射频消融术的房颤患者242例,术后3~12月随访期间,有209例患者未复发心房颤动,33例患者复发心房颤动。复发组术后应用β受体阻滞剂的比例高于未复发组,且差异有统计学意义(P < 0.05)。超声心动图指标方面,复发组LADi明显高于未复发组,且差异有统计学意义(P < 0.05)。余复发组与未复发组的年龄、性别、基础疾病、术后抗心律失常、抗凝药物的结果比较,差异均无统计学意义。见表1。

Table 1. Clinical data comparison in atrial fibrillation recurrence group and non-recurrence group
表1. 房颤复发组与未复发组患者的临床资料比较
3.2. 影响房颤复发的Logistic回归分析
对可能影响房颤患者射频消融术后复发的年龄、性别、基础疾病等危险因素进行logistics回归分析,结果显示,LADi为房颤短期复发的独立危险因素(OR = 1.251, 95% CI: 1.093~1.431, P = 0.001)。见表2。

Table 2. Logistic regression analysis of recurrence of atrial fibrillation after RFCA
表2. RFCA后房颤复发的logistic回归分析
3.3. ROC曲线分析
ROC曲线分析显示,LADi预测RFCA后房颤复发的曲线下面积为0.675 (95% CI: 0.579~0.771, P = 0.01),LADi取截断值为27.54时,其敏感度为0.606,特异度0.695。见图2。
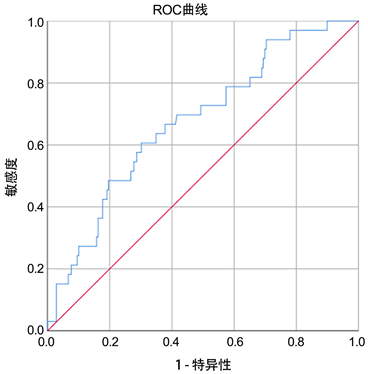
Figure 2. ROC curve of LADi predicting short-term recurrence after radiofrequency ablation in patients with atrial fibrillation
图2. LADi预测房颤患者射频消融术后短期复发的ROC曲线
4. 讨论
近年来研究表明,房颤患者射频消融术后复发,与术前左心房重构及重构的可逆性有关 [8]。测量左心房容积大小,可评估患者左心房重构程度,推荐的方法有左心房径线测量及左心房容积测量。但左心房容积测量方法繁琐,其结果易受左心房内膜是否显示清晰、扫查切面是否准确等因素的影响,仍不能广泛应用于临床。目前,左心房径线测量为临床上常用的评估左心房大小的指标。
考虑到左心房的容积存在空间性,且受体型、解剖位置等的影响,当左心房大小发生改变时,其左右径、前后径、上下径并非等比例变化,因此单一径线的测量往往不能准确反映左心房大小 [9]。本研究综合了多个径线,测量左心房前后径、左右径及上下径,并取其平均值(D)准确评价左心房大小,需要排除身高、体重等的影响 [10] [11] [12],本研究以体表面积标化左心房径线的平均值,得到左心房径线指数(LADi)。LADi不仅综合了三条径线,且消除了身高、体重等因素的影响,进一步提高了评估左心房大小的准确度。
本研究结果显示,房颤复发组的左心房径线指数明显高于房颤未复发组,且差异有统计学意义。经过logistic回归方程分析,左心房径线指数是RFCA后房颤复发的独立危险因素,ROC曲线分析显示左心房径线指数对RFCA后房颤复发有较高的预测价值。
本研究表明,左心房径线指数较大的患者在房颤消融后复发的风险较高,这种简便的非侵入性指标可为房颤患者术后管理和治疗提供可靠信息。但本研究尚存在一定局限性,为单中心研究,纳入样本量较少,降低了分析效能。在随访中,可能存在患者复发无症状房颤而未被观察和记录的情况,这可能对研究结果有一定影响。
NOTES
*通讯作者Email: qdtanlijuan@126.com