摘要: 目的:探讨不同中心凹内层视网膜异位(EIFL)分级的特发性黄斑前膜(IMEM)行玻璃体切除联合黄斑前膜内界膜剥除术后早期黄斑结构和视功能效果以及影响因素,并比较不用玻璃体腔填充物对手术疗效的影响。方法:收集2018年12月至2022年6月就诊于青岛大学附属医院眼科并确诊为IMEM的患者共51例(共51眼),根据患者术前光学相干断层扫描(OCT)图像,将EIFL2级、3级、4级IMEM患者分别纳入A组、B组、C组。收集三组患者的性别、年龄、病程、手术方式、手术前后最佳矫正视力(BCVA)、黄斑中心凹厚度(CFT)、黄斑容积、黄斑平均容积厚度、神经节细胞层(GCL)厚度,术后随访3个月,比较各组患者术后视网膜结构及视功能的差异,分析不同分级患者接受手术治疗后视网膜结构及视功能的改善效果及影响因素,探究不同玻璃体腔填充物对存在EIFL患者的手术效果的影响。结果:不同分级患者术后视力均较术前改善,A组、C组患者术后CFT厚度较术前降低,差异具有统计学意义(P < 0.05)。B组、C组手术前后黄斑容积及黄斑平均容积厚度均降低,差异具有统计学意义(P < 0.05),但各组术前–术后GCL厚度变化不明显。IMEM患者术前BCVA (log MAR)、EIFL分级与术后BCVA (log MAR)存在相关性。存在EIFL的患者术后玻璃体腔空气填充与否对术后黄斑结构及视功能的恢复差异并无统计学意义(P > 0.05)。结论:EIFL分级法对IMEM患者手术时机选择及预后判断具有一定指导作用,EIFL分级早、术前视力好的患者能够获得更好的视力预后。
Abstract:
Objective: To investigate the early effects and influencing factors of macular structure and visual function of idiopathic macular epiretinal membrane (IMEM) with different ectopic inner foveal lay-ers (EIFL) staging scheme after vitrectomy combined with ectopic inner foveal layer. Methods: A to-tal of 51 eyes of 51 patients diagnosed with IMEM in the Department of Ophthalmology, Affiliated Hospital of Qingdao University from December 2018 to June 2022 were collected. According to pre-operative optical coherence tomography (OCT) images, patients with EIFL-2, 3 and 4 IMEM were di-vided into group A, group B and group C, respectively. The gender, age, course of disease, surgical method, best corrected visual acuity (BCVA), foveal thickness (CFT), macular volume, macular mean volume thickness, and ganglion cell layer (GCL) thickness were collected before and after surgery, and the patients were followed up for 3 months. The differences in retinal structure and visual function were compared among the three groups. To analyze the improvement effect and influenc-ing factors of retinal structure and visual function in patients with different grades after surgical treatment and the effect of different intravitreal fillers on the surgical outcome of patients with EIFL. Results: The visual acuity of patients with different grades was improved after operation, be-sides, the CFT thickness of patients in group A and C was reduced compared with pre-operation, and the differences were statistically significant (P < 0.05). The macular volume and macular mean volume thickness of group B and C were decreased before and after operation, and the differences were statistically significant (P < 0.05), but the GCL thickness of each group before and after opera-tion did not change significantly. Preoperative BCVA (Log MAR), and EIFL grade were correlated with postoperative BCVA (Log MAR) in IMEM patients. There was no significant difference in the re-covery of macular structure and visual function in patients with EIFL (P > 0.05). Conclusion: EIFL grading has a certain guiding role in the selection of surgical timing and prognosis of patients with IMEM. Patients with early EIFL grading and good preoperative vision can obtain better vision prog-nosis.
1. 引言
特发性视网膜前膜(Idiopathic Epiretinal Membrane, IERM)是视网膜内表面的纤维细胞增生,在玻璃体视网膜界面形成的非血管性纤维增殖膜,当视网膜前膜发生于黄斑及其附近时,称为特发性黄斑前膜(idiopathic macular epiretinal membrane, IMEM)。黄斑区纤维增殖膜的收缩能导致视网膜形态改变,进而引起视网膜内外态结构与功能的改变 [1],最终导致视力下降,甚至中心视力丧失 [2]。光学相干断层扫描(optical coherence tomography, OCT)作为诊断黄斑疾病的金标准,许多指标被发现可以用于IMEM术后效果的预测,但由于测量方法困难或者图像质量较低,各种基于OCT图像预测患者预后的生物学标志物,应用到临床的普遍性受到限制。中心凹内层视网膜异位(ectopic inner foveal layer, EIFL)分级法 [3] 是Govetto基于内层视网膜结构角度提出的对IMEM新的分级标准:1级:轻度黄斑前膜,视网膜各层可识别,黄斑中心凹陷存在为主要特征;2级:黄斑前膜伴有黄斑中心凹消失及外核层增宽;3级:黄斑前膜伴有黄斑中心凹凹陷消失及EIFL,即连续且清晰识别的内核层(低反射带)和内丛状层(高反射带)穿过中心凹。4级:黄斑前膜较厚伴EIFL,各层视网膜结构无法辨认。本研究以EIFL分级法为基础,探讨不同EIFL分级IMEM患者术后早期黄斑结构及视功能的差异及影响因素,并分析不同玻璃体腔填充物对存在EIFL患者术后早期视功能恢复的影响,为IMEM患者选择最佳手术时机及手术方式提供理论基础。
2. 资料与方法
回顾性收集2018年12月~2022年6月就诊于青岛大学附属医院眼科并确诊为IMEM的患者的临床资料,所有患者均接受视力、非接触眼压计测量、散瞳后间接检眼镜检查、验光、眼部超声及OCT检查,根据以下标准进行筛选。纳入标准:① 首次就诊并主诉视力下降和(或)视物变形;② 经散瞳后间接检眼镜检查见黄斑区玻璃纸样反光及皱褶等黄斑前膜表现;③ OCT检查符合黄斑前膜的表现;④ EIFL分期 ≥ 2级,具有手术指征,临床资料完整。排除标准:① 既往有内眼手术史;② 视网膜脱离、视网膜裂孔等病史③ 任何原因造成的视网膜、脉络膜新生血管病史④ 青光眼等视神经病变;⑤ 既往视网膜动静脉阻塞导致的眼底出血病史⑥ 既往眼内感染或眼外伤病史。研究纳入患者共51例(51只眼),根据患者术前OCT检查所示的黄斑形态参考以下分级标准将研究对象分为A组(2级,13眼)、B组(3级,13眼)、C组(4级,25眼)。代表性黄斑区OCT图像见图1。

Figure 1. OCT images of different EIFL stages. (A) Stage 1 representative OCT image of macula; (B) Stage 2 representative OCT image of macula; (C) Stage 3 representative OCT image of macula; (D) Stage 4 representative OCT image of macula
图1. 不同EIFL分级的OCT扫描图像。(A) EIFL 1级代表性黄斑OCT图像;(B) EIFL 2级代表性黄斑OCT图像;(C) EIFL 3级代表性黄斑OCT图像;(D) EIFL 4级代表性黄斑OCT图像
所有患者均接受标准23G三切口经平坦部玻璃体切除联合黄斑前膜、内界膜剥除术,手术由同一经验丰富的术者实施,术后规律随访。收集每例患者性别、年龄、病程、玻璃体腔填充物、手术前后最佳矫正视力(BCVA)、黄斑中心凹厚度(Central foveal thickness, CFT)、神经节细胞层(Ganglion cell layer, GCL)厚度、黄斑容积和黄斑平均容积厚度。将BCVA转换为log MAR进行统计学分析。若术后BCVA高于术前视为视力提高,EIFL分级降低视为黄斑结构改善。对比各组患者手术前后各项指标的变化及相关性。
采用SPSS 22.0统计学软件进行数据分析。对计量资料进行Shapiro-Wilk检验,符合正态分布的数据以x ± s表示,使用单因素方差分析进行统计学检验。不符合正态分布的数据采用M(P25, P75)表示,使用Wilcoxon符号秩和检验、Kruskal-Wallis H检验进行差异性分析;计数资料采用百分比表示,使用χ2检验或Fisher精确检验进行统计学分析。进行Pearson、Spearman相关性分析,P < 0.05认定为具有统计学意义。
3. 结果
3.1. 患者基本资料
符合标准的有51例(51只眼)被纳入本研究并进行统计学分析,男18例,女33例,年龄49~75岁,平均年龄(65.02 ± 6.36)岁,病程为0.2~96个月,平均病程(23.10 ± 23.89)月,3组间患者年龄、性别、病程比较差异无统计学意义(P > 0.05),见表1。

Table 1. Comparison of preoperative basic factors in each group
表1. 各组患者术前基本因素比较
3.2. 不同组内患者术后视力及黄斑结构恢复情况
每组患者接受手术治疗后BCVA较术前均有改善,差异具有显著性(P < 0.05),见表2。A组患者视力提高率为92.31%,B组患者视力提高率为84.62%,C组患者视力提高率为68%,三组视力提高率较术前差异具有统计学意义(χ2 = 7.761, P < 0.05)。手术治疗后各组患者CFT较术前变薄,其中A组差异具有统计学意义(P < 0.05),A组、B组黄斑容积及黄斑平均厚度较术前降低,差异具有显著性(P < 0.05)。3组治疗前后GCL厚度差异无统计学意义(P > 0.05)。

Table 2. Comparison of visual acuity and macular parameters before and after operation
表2. 各组患者手术前后视力及黄斑参数比较
注:a:配对样本Wilcoxon符号秩和检验;b:配对样本t检验。
3.3. 不同组间患者术后视力及黄斑结构恢复情况
IMEM患者术后视力A组(0.75 ± 0.13),B组(0.55 ± 0.18),C组(0.40 ± 0.23),差异具有统计学意义(F = 0.767, P < 0.85),黄斑容积A组(10.63 ± 1.56 μm)、B组(12.10 ± 1.01 μm)、C组(12.73 ± 1.54 μm),差异具有统计学意义(F = 5.815, P < 0.05),黄斑平均容积厚度A组(295.38 ± 42.92 μm),B组(336.33 ± 28.13 μm),C组(353.31 ± 42.62 μm),差异具有统计学意义(F = 5.791, P < 0.05),平均神经节细胞厚度A组(64.00 ± 17.79 μm),B组(39.11 ± 14.44 μm),C组(44.77 ± 18.08 μm),差异具有统计学意义(F = 4.575, P < 0.5)。
3.4. IMEM患者术后术眼BCVA相关性分析
将因变量定位患者术后术眼BCVA,记为LogMAR,分别选取病程、年龄、术眼黄斑各项参数为自变量并绘制散点图,见图2~4,进行相关分析,以P < 0.05认为差异具有统计学意义。通过分析可知患者术后LogMAR与术前LogMAR、术前EIFL分级与术前CFT呈正相关(P < 0.05)。

Figure 2. Scatter plot of preoperative LogMAR versus postoperative LogMAR in IMEM patients
图2. IMEM患者术前LogMAR与术后LogMAR的散点图
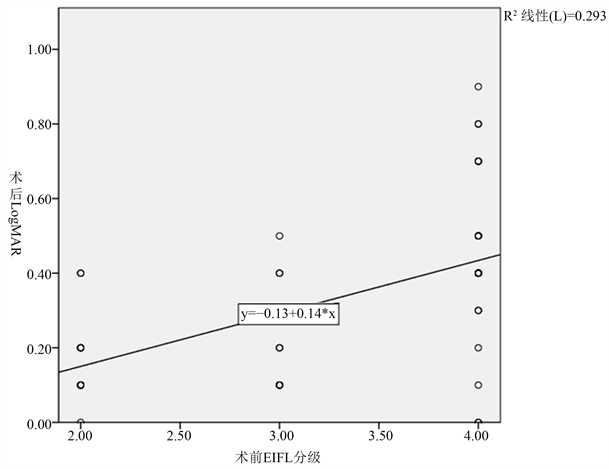
Figure 3. Scatter plot of preoperative EIFL grade and postoperative LogMAR in IMEM patients
图3. IMEM患者术前EIFL分级与术后LogMAR的散点图

Figure 4. Scatter plot of preoperative CFT and postoperative LogMAR in IMEM patients
图4. IMEM患者术前CFT与术后LogMAR的散点图
3.5. Logistic回归分析
将上述具有统计学意义的术前因素与术后log MAR进行Logistic回归分析,见表3,结果显示Log MAR、EIFL分级与术后log MAR呈正相关,差异具有统计学意义(P < 0.05)。

Table 3. Logistic regression analysis of preoperative factors in IMEM patients
表3. IMEM患者术前因素Logistic回归分析
3.6. 玻璃体腔空气填充与平衡盐填充对存在EIFL患者术后视力及黄斑结构的影响
无EIFL组(A组)和存在EIFL组(B组、C组)二者空气填充率分别为23.08%,31.58%,组间差异无统计学意义(χ2 = 0.052, P > 0.05)。两组术后BCVA、CFT差异无统计学意义(P > 0.05)。
4. 讨论
IMEM是玻璃体黄斑界面在视网膜上的切向牵引力导致视网膜结构变形的一种玻璃体视网膜交界面疾病 [4],患病率为7%~11.8%,其中年龄增长是最重要的危险因素 [5],有报道称,年龄每增加10岁,患病风险将增加1.2倍~1.5倍 [6]。其发病机制是多因素的,导致视力丧失的机制较为复杂,目前尚未完全了解,黄斑正常凹陷结构有利于光线经过折射直接刺激感光细胞,是良好视功能的保障。随着OCT扫描技术的发展,可以直接获得各层视网膜和玻璃体视网膜界面结构的清晰图像,有助于能够更好地了解黄斑疾病在手术前后的形态学变化 [7],对评估术后视力具有参考意义。到目前为止,许多研究报告了OCT图像能够提供预测IMEM患者预后的生物学特征,如:没有EIFL、内层视网膜不规则、黄斑囊样水肿或获得性卵黄样病变、EZ带和COST线的完整性和术前更薄的神经节细胞层–内丛状层 [8] [9] [10] [11] [12]。但由于测量方法及图像质量的限制,一些特征在临床应用上具有限制性。EIFL分级是Govetto继Gass分级之后提出的一种相对简单、快速及重复性较高的方法,与Gass分级通过直接观察黄斑形态预测患者预后相比,EIFL分级方案增加了OCT层面上对黄斑精细结构的了解。因此本研究基于EIFL分级法,通过分析IMEM患者的临床资料,探究不同分级患者经玻璃体切除手术的治疗效果及相关因素。
一般情况下,IMEM最初是无症状的,症状的发展取决于IMEM的位置、持续时间、严重程度和类型。在某些情况下,疾病进展到黄斑或黄斑周围区域受累、视网膜牵拉、水肿、纤维膜增厚时,视功能可能会受到影响,目前无法尚无有效保守治疗方法,当患者出现低视力、严重视物变形时需要采取手术干预疾病进展 [13]。有研究表明,术前视网膜厚度可能是视觉增益的重要预测因素。在本次研究中,我们发现各分级患者接受手术治疗后,CFT较术前均有减少,A组、C组患者手术前后CFT厚度差值具有统计学意义(P < 0.05)。术前较薄的GCL层厚度代表具有更多改善能力的受损组织,被认为是IMEM患者术后BCVA改善的预后因素 [14],但在本研究中,随着EIFL分级增加,GCL层厚度逐渐降低,术后各组GCL厚度较术前差异无统计学意义(P > 0.05),我们猜想由于IMEM进展缓慢,IMEM对黄斑区视网膜的长期牵拉导致内层视网膜受损,玻璃体手术虽然解除了IMEM对黄斑区的牵引力,但牵拉导致的细胞水肿或细胞间水肿短期内无法改善,可能作为IMEM患者术后早期视力较差的原因之一。
手术解除黄斑区纤维增殖膜的牵引力仍是目前安全有效治疗方法。平坦部玻璃体切除术与ERM剥离术能够释放IMEM对视网膜的牵引力,被认为是维持视力、维持视网膜解剖结构和功能的标准治疗方案 [15],但术后并不总能达到预期的视觉效果,并且视网膜形态结构及功能恢复至正常所需时间不同,并不是完全都可以恢复,因此手术干预的最佳时机备受争议。在本次研究中,三组患者术后BCVA较术前明显提高,但C组患者无论是术前或术后视力,与A组、B组相比普遍较差,相关性分析显示IMEM患者术前BCVA (log MAR)、CFT、EIFL分级与术后BCVA (log MAR)存在相关性(P < 0.05)。综上所述,在IMEM发生的各个阶段进行手术治疗均可显著提高视功能,但早期接受玻璃体切除手术解除增殖膜对黄斑部位的牵引,对IMEM患者术后视功能获益最大。
玻璃体视网膜手术已经成为一种被广泛接受的技术,由于黄斑手术中器械的微创特性、技术进步以及更快的术后康复在日益普及中发挥了重要作用 [16] [17] [18],眼科医生会根据术中情况决定手术结束时的玻璃体腔内填塞物。作为玻璃体切除后玻璃体腔填塞材料的空气会暂时停留在眼内空间,直到被组织液替换,相较C3F8等气体填充物能够造成继发性眼压升高和继发性白内障 [19],空气填充持续时间更短,更为安全。在玻璃体视网膜界面疾病的治疗中,空气作为常用的眼内填充物之一,因为无视网膜毒性,短期内自行吸收,可减少术后低头时间,与眼内平衡盐溶液填充相比,能有效使黄斑结构恢复 [20] [21],进而提高视力。但另有研究指出,IMEM患者术中使用空气填充物与否在术后视网膜解剖及功能效果方面没有显著差异 [22] [23]。因此我们研究了存在EIFL与不存在EIFL患者玻璃体腔内空气使用率差异并无统计学意义(χ2 = 0.052, P > 0.05)。玻璃体腔空气填充较平衡盐填充患者视力差异无统计学意义(P > 0.05),部分患者术后OCT图像显示视网膜结构的改善,但差异并无显著性,我们猜想,虽然眼内过滤空气的短期填充能够促进视网膜内水肿的消退及视网膜结构的恢复,但对最终矫正视力无明显优势,可能与高分级IMEM患者术后黄斑水肿风险增加有关 [24],推断IMEM手术的最佳时间可能是在EIFL发展之前。
本次研究存在一定的不足之处,回顾性研究会存在一定的选择偏倚,受患者依从性限制,无法进行大样本、前瞻性研究,同时IMEM进展相对缓慢的疾病,因此更大的样本量、更长的随访时间动态观察患者手术治疗效果更为客观准确。
综上所述,尽管IMEM引起视力损害的机制尚不清楚,但EIFL分级法对于判断手术时机及预后具有一定的指导意义,玻璃体腔空气填充与否对于有EIFL眼术后黄斑结构及视功能的治疗效果不明显,因此术中应根据情况选择合适的眼内填充物促进IMEM患者视网膜结构及功能的恢复。
基金项目
山东省自然科学基金,编号ZR2017MH055,PTP1B调节RPE细胞信号转导在增殖性玻璃体视网膜病变中的作用研究;国家自然科学基金,编号81900824,Candidalysin调控TREM-1/DAP12触发真菌性角膜炎免疫炎症反应的分子机理研究;青岛市中医药科研计划项目,编号2020-zyy052。
伦理批准和知情同意
本研究涉及的所有试验均已通过青岛大学附属医院医学伦理委员会的审核批准(QYFY WZLL 27322)。所有试验过程均遵照《赫尔辛基宣言》的条例进行。受试对象或其亲属已签署知情同意书。
NOTES
*通讯作者Email: duzhaodong@126.com