摘要: 目的:研究早期液体复苏入量及相关临床指标包括血尿素氮(BUN)、乳酸清除率(LCR)、下腔静脉变异度(IVCV)及急性生理与慢性健康(APACHE II)评分、序贯器官衰竭估计(SOFA)评分对老年脓毒性休克患者预后评估价值。方法:研究纳入2020年10月至2023年10月青岛市市立医院东院区收治的70例老年脓毒性休克患者,根据患者28天预后结果分为存活组(34例,48.6%)和死亡组(36例,51.4%),比较两组患者入院时的一般资料及入院6 h时的液体复苏入量、LCR、IVCV及入院24小时内APACHE II评分、SOFA评分,应用二元Logistic回归分析法分析影响老年脓毒性休克患者28天预后的独立危险因素,并绘制受试者工作特征(ROC)曲线,评估各指标对老年脓毒性休克患者28天预后的评估价值。结果:死亡组的BUN、APACHE II评分、SOFA评分高于存活组,6 h LCR低于存活组,且死亡组入院6 h无下腔静脉变异度(完全机械通气患者IVCV < 18%或自主呼吸患者IVCV < 50%)的患者明显多于存活组(P < 0.05)。死亡组患者在入院6小时内接受了更多的液体入量(P < 0.05)。应用二元Logistic回归分析校正了年龄、性别、BMI、白蛋白、CRP、PCT、基础疾病等混杂因素后,结果显示BUN (OR = 1.087, P < 0.05)、6 h LCR (OR = 0.983, P < 0.05)、6 h IVCV (OR = 15.557, P < 0.01)、APACHE II评分(OR = 1.175, P < 0.01)、SOFA评分(OR = 1.586, P < 0.01)、及入院6 h液体复苏入量(OR = 1.001, P < 0.05)均是影响老年脓毒性休克患者死亡的独立危险因素。绘制ROC曲线分析显示BUN、6 h LCR、APACHE II评分、SOFA评分、6 h液体复苏入量对老年脓毒性休克患者28天预后均有一定预测价值(P < 0.05)。其中APACHE II评分(AUC = 0.737, Cut-off = 26.50, P < 0.01)、SOFA评分(AUC = 0.735, Cut-off = 9.50, P < 0.01)预测老年脓毒性休克患者28天预后的AUC高于其他指标,低于四者联合指标(AUC = 0.785, P < 0.01)。上述六个指标联合对老年脓毒性休克患者28天预后的预测价值最好(AUC = 0.824, P < 0.01)。结论:入院6 h液体复苏入量、BUN、6 h LCR、6 h IVCV及APACHE II评分、SOFA评分均是影响老年脓毒性休克患者28天死亡的独立危险因素。在老年脓毒性休克患者液体复苏治疗时,不宜短时间内摄入过多液体(最佳截断值为1042.50 mL,灵敏度为72.2%,特异度为55.9%)。入院6 h液体复苏入量、BUN、6 h LCR、6 h IVCV及APACHE II评分、SOFA评分六项指标联合对老年脓毒性休克患者28天预后预测价值最高。
Abstract:
Objective: Research on early fluid resuscitation volume and associated clinical indicators involves blood urea nitrogen (BUN), lactate clearance rate (LCR), inferior vena cava variability (IVCV), acute physiology and chronic health evaluation II (APACHE II) score, sequential organ failure assessment (SOFA) score for prognostic assessment in elderly patients with septic shock. Methods: The study included 70 elderly septic shock patients admitted in the East Hospital District of Qingdao Municipal Hospital from October 2020 to October 2023. According to the 28-day prognosis of patients, they were divided into survival group (34 cases, 48.6%) and death group (36 cases, 51.4%), Compare the general information of two groups of patients upon admission, as well as the fluid resuscitation volume, LCR, IVCV at 6 hours of admission, and APACHE II and SOFA scores within 24 hours of admission, the application of binary logistic regression analysis to analyze the independent risk factors affecting the 28-day prognosis of elderly patients with septic shock, and plot the working characteristics of the subjects (ROC) curve to evaluate the evaluation value of each indicator for the 28-day prognosis of elderly patients with septic shock. Results: The BUN, APACHE II and SOFA scores in the death group were higher than those in the survival group, 6 h LCR was lower than in the survival group, and the patients who were admitted to the death group for 6 hours without inferior vena cava variation (IVCV < 18% in patients with complete mechanical ventilation or IVCV < 50% in patients with autonomous breathing) were obvious, more than the surviving group (P < 0.05). The patients in the dead group received more fluid intake (P < 0.05) within 6 hours of admission. After applying binary logistic regression analysis to correct age, gender, BMI, albumin, CRP, PCT, basic diseases and other mixed factors, the results showed BUN (OR = 1.087, P < 0.05), 6 h LCR (OR = 0.983, P < 0.05), 6 h IVCV (OR = 15.557, P < 0.01), APACHE II score (OR = 1.175, P < 0.01), SOFA score (OR = 1.586, P < 0.01), and admission 6 h liquid resuscitation input (OR = 1.001, P < 0.05) are independent risk factors affecting the death of elderly patients with septic shock. The ROC curve analysis shows that BUN, 6 h LCR, APACHE II score, SOFA score, and 6 h fluid resuscitation input have a certain predictive value for the 28-day prognosis of elderly patients with septic shock (P < 0.05). Among them, The APACHE II score (AUC = 0.737, Cut off = 26.50, P < 0.01) and SOFA score (AUC = 0.735, Cut off = 9.50, P < 0.01) predict a higher AUC than other indicators for the 28-day prognosis of elderly patients with septic shock, and lower the four combined indicators (AUC = 0.785, P < 0.01). The combination of six indicators has the best predictable value for the 28-day prognosis of elderly patients with septic shock (AUC = 0.824, P < 0.01). Conclusion: 6 h liquid resuscitation intake, BUN, 6 h LCR, 6 h IVCV and APACHE II scores, and SOFA scores are all independent risk factors affecting the 28-day death of elderly patients with septic shock. In the treatment of fluid resuscitation in elderly patients with septic shock, it is not appropriate to ingest too much fluid in a short period of time (the optimal truncation value is 1042.50 mL, the sensitivity is 72.2%, and the specificity is 55.9%). Six indicators of admission 6 h liquid resuscitation input, BUN, 6 h LCR, 6 h IVCV and APACHE II score, and SOFA score have the highest prognostic value for 28 days of elderly patients with septic shock.
1. 引言
根据脓毒症和脓毒性休克第三个国际共识(Sepsis-3),脓毒症是因感染引起的宿主反应失调所致的危及生命的器官功能障碍 [1] [2] 。当脓毒症患者采用积极的液体复苏治疗后,仍然需要使用血管活性药物使平均动脉压维持在 ≥ 65 mmHg,且血乳酸 > 2 mmol/L,即可诊断脓毒性休克 [2] ,是导致脓毒症死亡的主要原因 [3] 。脓毒症的发病率和死亡率随着年龄的增长而显著增加 [4] 。研究表明,超过60%的脓毒症患者的年龄大于65岁 [5] ,且老年脓毒症患者的死亡率明显高于成年患者 [6] [7] 。早期液体复苏作为脓毒性休克治疗的核心措施之一 [8] ,一直是研究的重点内容。越来越多的研究表明,液体补充量不足或过量均会影响患者预后,导致死亡率增加 [9] [10] 。由于老年人存在免疫抑制、器官老化、合并有多种基础疾病以及营养不良等问题 [11] ,对于老年脓毒性休克患者如何进行液体复苏尚未有明确定论。本研究是一项单中心回顾性研究,期望通过研究影响老年脓毒性休克患者预后的危险因素,及早期液体复苏入量特点,为临床评估患者预后提供更好、更全面的监测指标,更好地指导早期液体复苏。
2. 资料与方法
2.1. 研究对象
选取2022年10月至2023年10月我院收治的符合标准的70例老年脓毒性休克患者。其中纳入标准:(1) 依据《脓毒症和脓毒性休克定义的第三次国际共识(sepsis-3.0)》中脓毒性休克诊断标准,符合脓毒性休克的诊断;(2) 年龄 ≥ 65岁;排除标准:(1) 年龄 < 65岁;(2) 伴有免疫系统疾病或长期应用免疫抑制类药物的患者;(3) 因心源性休克、失血性休克、严重心血管疾病、急性心肌梗死等非脓毒症原因死亡的患者;(4) 伴有血液病、恶性肿瘤、慢性器官衰竭终末期(如肝衰竭)等可能影响预后的患者;(5) 放弃治疗、住院时间不满足24小时、临床资料不完整者;符合一项即可排除在外。本研究已获得青岛市市立医院医学伦理委员会批准。
2.2. 研究方法
本研究是一项观察性研究,纳入研究的患者入院后行重症监护,监测患者的生命体征,尽早开始液体复苏治疗。根据患者实际临床症状及感染病种,为患者展开抗感染、血管活性药物、呼吸支持及机械通气、床旁肾脏替代等治疗。并在患者入院6 h时测量下腔静脉变异度(IVCV)计算患者入院6小时液体复苏入量及乳酸清除率(LCR)。床旁超声测量IVCV时患者取平卧位,找到剑突下下腔静脉纵切面,取下腔静脉距离右心房入口2 cm处,在M模式下测量呼气时最大直径(IVCmax)、吸气时最小直径(IVCmin),并计算VIVC = (IVCmax − IVCmin)/IVCmax × 100%,测量3次取平均值,认为完全机械通气患者IVCV < 18%或自主呼吸患者IVCV < 50%无下腔静脉变异度 [12] 。6 h乳酸清除率(6 h LCR) = (初始乳酸值 − 6 h复测乳酸值)/初始乳酸值 × 100% [13] 。并收集各患者入院时的一般临床资料,包括年龄、性别、基础疾病、及首次临床化验指标、入院24小时内的急性生理与慢性健康(APACHE II)评分、序贯器官衰竭估计(SOFA)评分。根据患者入院28天结局,将患者分为存活组及死亡组,对两组数据进行统计学分析。
2.3. 统计分析方法
采用spss26.0软件对各项数据进行统计学分析。采用Shapiro-wilk检验检测计量资料否符合正态分布。服从正态分布和方差齐性的计量资料采用均值 ± 标准差(
)表示,两组间比较采用独立样本t检验;不服从正态分布和方差齐性的计量资料采用四分位数M(P25, P75)表示,组间比较采用非参数检验(Mann-Whitney U检验)。计数资料采用例数/百分比(n/%)表示,组间比较采用χ2检验。采用二元Logistic回归分析法分析老年脓毒性休克患者28天死亡的影响因素,并用ROC曲线判定影响因素指标对预后的预测价值。以P < 0.05表示差异具有统计学意义。
3. 结果
3.1. 一般资料比较
本研究共纳入老年脓毒性休克患者70例,其中入院28天存活34例(48.6%),死亡36例(51.4%),男性37例(52.9%),女性33例(47.1%),年龄79.50 (71.75, 84.00)岁。根据患者入院28天预后将70例患者分为存活组及死亡组。分别比较存活组及死亡组的入院时一般临床资料,结果显示死亡组的BUN高于存活组(P < 0.05),两组患者的性别、年龄、BMI、血糖、BNP、ALT、AST、白蛋白、肌酐、CRP、PCT、基础疾病(包括高血压、糖尿病、冠心病、慢性肺病、慢性肾脏病)患病率,差异均无统计学意义(P > 0.05)。见表1。

Table 1. Comparison of two sets of general information
表1. 两组一般资料比较
注:BMI为身体质量指数;BNP为B型脑钠肽;ALT为丙氨酸氨基转移酶;AST为天门冬氨酸氨基转移酶;BUN为血尿素氮;CRP为C反应蛋白;PCT为降钙素原。
3.2. 两组监测数据比较
对两组患者各监测指标进行分析,结果显示死亡组的6 h LCR低于存活组,APACHE II评分、SOFA评分高于存活组,且死亡组入院6 h无下腔静脉变异度(IVCV)的患者明显多于存活组,差异均有统计学意义(P < 0.05)。在对老年脓毒性休克患者入院6 h液体复苏入量分析可以看出,死亡组患者在入院6小时内接受了更多的液体入量,差异有统计学意义(P < 0.05)。见表2。

Table 2. Comparison of two monitoring indicators
表2. 两组监测指标比较
3.3. 老年脓毒性休克患者28天预后影响因素的二元Logistic回归分析
应用二元Logistic回归分析校正了年龄、性别、BMI、白蛋白、CRP、PCT、基础疾病等混杂因素后,结果显示BUN (OR = 1.087, P < 0.05)、6 h LCR (OR = 0.983, P < 0.05)、6 h IVCV (OR = 15.557, P < 0.01)、APACHE II评分(OR = 1.175, P < 0.01)、SOFA评分(OR = 1.586, P < 0.01)及入院6 h液体复苏入量(OR = 1.001, P < 0.05)均是影响老年脓毒性休克患者死亡的独立危险因素。见表3。
3.4. 各指标对老年脓毒性休克患者预后的预测价值
通过绘制ROC曲线分析BUN、6 h LCR、6 h IVCV、APACHE II评分、SOFA评分及入院6 h液体复苏入量以及联合指标对老年脓毒性休克患者28天预后的预测价值。结果显示BUN、6 h LCR、APACHE II评分、SOFA评分、6 h液体复苏入量对老年脓毒性休克患者28天预后均有一定预测价值(P < 0.05)。其中APACHE II评分(AUC = 0.737, P < 0.01)、SOFA评分(AUC = 0.735, P < 0.01)预测老年脓毒性休克患者28天预后的AUC高于BUN (AUC = 0.645, P < 0.05)、6 h LCR (AUC = 0.677, P < 0.05)及6 h液体复苏入量(AUC = 0.649, P < 0.05),低于BUN、6 h LCR、6 h IVCV、6 h液体复苏入量四者联合指标(AUC = 0.785, P < 0.01)。六个指标联合(BUN、APACHE II评分、SOFA评分、6 h LCR、6 h IVCV、入院6 h液体复苏入量)对老年脓毒性休克患者28天预后的预测价值最好(AUC = 0.824, P < 0.01)。见表4,图1、图2。

Table 3. Factors affecting the 28 day prognosis of elderly patients with septic shock
表3. 老年脓毒性休克患者28 d预后影响因素

Table 4. The predictive value of various indicators on the 28 day prognosis of elderly patients with septic shock
表4. 各指标对老年脓毒性休克患者28 d预后的预测价值
注:模型1指BUN、6 h LCR、6 h IVCV、6 h液体复苏入量联合指标。
4. 讨论
全世界每年有超过3000万例脓毒症患者,脓毒症发病率每年增加9%~13%,死亡率为33%~35% [14] 。一项关于我国ICU脓毒症及脓毒性休克发病率与死亡率的研究显示 [15] ,脓毒症的发病率为33.6%,脓毒症及脓毒性休克的总体死亡率分别是29%和37.3%。多项研究显示,在老年人群中,脓毒症及脓毒性休克具有更高的发病率与死亡率 [5] 。本研究共纳入70例老年脓毒性休克患者,其中36例(51.4%)患者在入院28天内死亡,明显高于一般人群,在当今老龄化社会,更加需要研究和关注。
脓毒性休克是一种分布性休克,它是全身血管广泛舒张、毛细血管通透性增高、液体渗漏至第三间隙导致的血管内容量绝对或相对不足 [16] [17] ,心脏前负荷、心室舒张末压、心输出量和全身氧输送急剧降低,导致的低血压和器官灌注不足 [18] 。所以,早期液体复苏尽快纠正血管内有效容量不足,保证器官组织灌注是治疗脓毒性休克的关键。自2001年Rivers [19] 等人提出早期目标导向治疗(EGDT)以来,关于
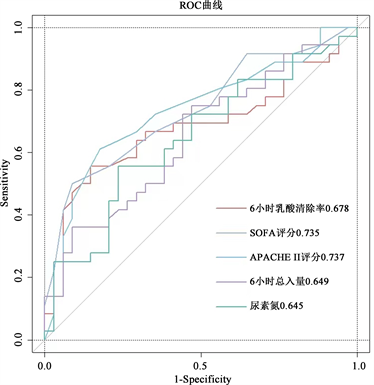
Figure 1. ROC curve of 28 day prognosis in elderly patients with septic shock using single factor indicators
图1. 单因素指标老年脓毒性休克患者28 d预后的ROC曲线

Figure 2. ROC curve of 28 day prognosis in elderly patients with septic shock using a combination of multiple indicators
图2. 多指标联合对老年脓毒性休克患者28 d预后的ROC曲线
脓毒性休克液体复苏的研究从未中断。2021年重症脓毒症及脓毒性休克管理国际指南建议 [1] ,对于成人患者在复苏的前3小时内给予至少30 mL/kg的静脉晶体液,但这一建议被列为“低质量”推荐。
老年人存在免疫抑制、器官老化、合并有多种基础疾病以及营养不良等问题 [7] [11] [20] 。老年人的器官老化,即器官功能减退,主要表现在心、肾、脑、肺等器官。与液体调节密切相关的器官主要是肾脏、心血管。心脏老化的特征是心肌细胞肥大或明显丢失,进而导致心肌功能障碍。随着年龄的增长,可引起心血管系统的结构和功能改变,如心室舒张功能减退、心肌收缩力减弱等 [21] 。肾脏老化征是肾小球硬化、肾小管萎缩及小动脉硬化,这种整体肾小球硬化导致肾单位持续丢失进而引起肾小球滤过率的下降 [22] 。正是因为老年人这些病理生理特征,使得老年患者如果按照指南推荐意见在3小时内摄入30 mL/kg的静脉晶体液体进行复苏,不但不能有效改善患者预后,反而加重脏器负担,增加发生肺水肿、急性心力衰竭,甚至MODS的风险 [23] [24] 。本研究结果显示,入院6 h液体复苏入量(OR = 1.001, P < 0.05)是影响老年脓毒性休克患者28天死亡的独立危险因素,通过对ROC曲线分析可以发现,6 h液体复苏入量(AUC = 0.649,Cut-off = 1042.50,灵敏度为72.2%,特异度为55.9%,P < 0.05)对老年脓毒性休克患者28天死亡有一定的预测价值,且最佳截断值为1042.50 mL,这个数值远低于指南推荐量,安全摄入量需大量数据及前瞻性研究进一步分析。老年脓毒性休克患者在早期液体复苏治疗中,不宜盲目按照指南推荐的30 mL/kg的液体量进行复苏,应通过监测临床各项指标来进行液体复苏。
血尿素氮(BUN)是人体蛋白质代谢的主要终产物,主要通过肾脏排出。当机体蛋白质过量分解或肾小球滤过率降低时,BUN水平将升高 [25] 。所以,BUN水平可以反映人体内蛋白质的分解代谢水平,也是肾功能损害的标志。脓毒症及脓毒性休克患者处于高蛋白分解代谢状态,且常并发急性肾损伤 [26] ,同时老年人常合并慢性肾脏病、肾功能不全等疾病。这些因素均可导致老年脓毒症及脓毒性休克患者BUN水平升高。李旭 [27] 等人的研究表明,BUN是影响患者预后的独立危险因素,以41.1 mg/dL作为BUN的临界值,患者的死亡风险有显著差异。本研究也表明,BUN (OR = 1.087, P < 0.05)是影响老年脓毒性休克患者28天死亡的独立危险因素,同时BUN (AUC = 0.645, Cut-off = 17.98, P < 0.05)最佳截断值为17.98 mmol/L,灵敏度为55.6%,特异度为76.5%,对老年脓毒性休克患者28天死亡有一定的预测价值。
乳酸是组织在缺氧状态糖酵解过程中的代谢产物。当机体受到氧代谢障碍、组织灌注受损、先天性代谢障碍、药物、毒素等因素影响时乳酸的生成会增加 [28] 。当发生脓毒性休克时,组织灌注不足,使乳酸生成增加,有效循环血量不足使乳酸排出减少。乳酸作为衡量脓毒症、脓毒性休克患者病情严重程度指标之一 [29] ,受到临床及研究的广泛关注。越来越多的研究表明 [30] [31] ,初始乳酸水平越高、6 h LCR越低,脓毒症患者28天死亡风险越高,这与本研究的结果相一致。本研究表明,6 h LCR (OR = 0.983, P < 0.05)是影响老年脓毒性休克患者28天死亡的独立危险因素,通过对ROC曲线分析可以发现,6 h LCR (AUC = 0.677, Cut-off = 4.56, P < 0.05)最佳截断值为4.56%,灵敏度为55.6%,特异度为85.3%,对老年脓毒性休克患者28天死亡有一定的预测价值。
下腔静脉(IVC)的直径受血容量、吸气和呼气时胸腔内压力变化的影响 [32] 。当患者吸气时,胸腔内负压增加,下腔静脉回流至右心的血量增加,使得下腔静脉直径减小。当患者呼气时,胸腔内负压降低,下腔静脉回流至右心的血量减少,下腔静脉直径增加。在老年脓毒性休克患者中,有效循环血量不足,回心血量减少,影响下腔静脉随呼吸变化,经早期液体复苏改善循环后,情况会有改善。下腔静脉直径的呼吸变化可以作为液体反应性指标 [33] 。本研究表明,6 h IVCV (OR = 15.557, P < 0.01)是影响老年脓毒性休克患者28天死亡的独立危险因素,当老年脓毒性休克患者入院6 h无下腔静脉变异度时(即完全机械通气患者IVCV < 18%或自主呼吸患者IVCV < 50%),提示患者液体反应性及调节性下降,预后不良,死亡风险高。
对影响老年脓毒性休克患者28天死亡的危险因素指标绘制受试者工作特征(ROC)曲线,对于单一指标来说,APACHE II评分(AUC = 0.737, Cut-off = 26.50, P < 0.01)、SOFA评分(AUC = 0.735, Cut-off = 9.50, P < 0.01)对老年脓毒性休克患者28天预后的预测价值最好。但是脓毒性休克作为一种复杂疾病,单一指标对患者预后的预测价值有限,建议多指标、多方面评估患者预后。本研究表明,将入院6 h液体复苏入量、入院时BUN及6 h LCR、6 h IVCV四项指标联合(AUC = 0.785, P < 0.01),再与APACHE II评分、SOFA评分六项联合(AUC = 0.824, P < 0.01)评估老年脓毒性休克患者28天预后效果更好。
5. 结论
入院6 h液体复苏入量、BUN、6 h LCR、6 h IVCV及APACHE II评分、SOFA评分均是影响老年脓毒性休克患者28天死亡的独立危险因素。在老年脓毒性休克患者早期液体复苏治疗时,不宜短时间内摄入过多液体(最佳截断值为1042.50 mL,灵敏度为72.2%,特异度为55.9%)。入院6 h液体复苏入量、BUN、6 h LCR、6 h IVCV及APACHE II评分、SOFA评分对老年脓毒性休克患者28天预后均有一定预测价值,六项指标联合预测价值最高,临床上可以通过早期监测上述指标来评估患者预后。
参考文献
NOTES
*通讯作者。