1. 引言
嗅觉是胎儿在系统发育中最早成熟的感官,新生儿出生后可识别不同的气味,不同气味的嗅觉干预能引起新生儿生理和行为状态的变化 [1]。母乳源自母亲,对新生儿具有先天的吸引特性,因此新生儿更喜欢母乳气味 [2]。母乳嗅觉刺激是借助棉垫、棉球或气味扩散器将母乳气味通过新生儿的嗅觉通路传导至大脑皮层,从而发生嗅觉反应 [3] [4] [5]。既往研究表明母乳嗅觉刺激可缓解新生儿操作性疼痛,提高吮吸效率,缩短达经口喂养过渡时间,减少呼吸暂停的发生 [6] [7] [8]。但大部分研究样本量较小,研究结果存在分歧,因此,本研究对母乳嗅觉刺激在新生儿护理中的文献进行meta分析,系统评价母乳嗅觉刺激的临床效果,旨在为临床护理实践提供理论依据。
2. 资料与方法
2.1. 纳入与排除标准
纳入标准:1) 研究类型:国内外公开发表的随机对照试验,无论是否采用盲法,文种限为中文和英文。2) 研究对象:出生日龄小于28天的新生儿。3) 护理措施:干预组是新生儿常规护理中加母乳气味进行嗅觉刺激,对照组是新生儿常规护理或使其暴露于无菌水或配方奶气味中。4) 结局指标:对疼痛的影响(疼痛评分、血氧饱和度、心率、哭闹持续时间),对喂养的影响(达经口喂养过渡时间、出院时体重)。排除标准:1) 干预措施是母乳嗅觉刺激联合其他干预措施。2) 数据无法转换为评价指标或数据信息不完整。3) 重复发表或以多种语言发表的文献。
2.2. 检索策略
计算机检索从建库至2021年11月期间PubMed、Embase、Web of Science、Cochrane Library、中国生物医学文献数据库、中国知网、维普和万方数据库中有关母乳嗅觉刺激在新生儿护理中应用效果的随机对照试验。英文检索式:(“infant*” or “newborn*” or “neonate*” or “premature*”) and (“human milk” or “breast milk*” or “maternal milk”) and (“odour*” or “smell” or “scent” or “olfactory stimulateon”);中文检索式:(“新生儿”or“足月儿”or“早产儿”) and (“母乳气味”or“嗅觉刺激”or“嗅觉安抚”)。检索策略采用主题词、自由词、截词检索及布尔逻辑运算符连接相结合的方式,同时追溯纳入文献的参考文献。
2.3. 文献筛选与资料提取
由2名研究者按照纳入和排除标准独立检索、筛选文献、提取数据后交叉核对,遇见分歧时通过讨论或由第3名研究者的意见决定。数据提取内容包括:一般信息(作者姓名及发表年份)、研究对象信息(样本量、胎龄)、干预措施及结局指标。
2.4. 文献质量评价
由2名研究者按照Cochrane手册5.1.0评价标准 [9] 对纳入文献进行质量评价。评价内容包括:随机序列的产生、分配隐藏、参与者及研究者盲法、结果评价者盲法、结果数据完整、选择性报道及其他偏倚。若完全符合以上标准,质量等级为“A”;部分符合以上标准,质量等级为“B”;完全不符以上标准,质量等级为“C”。
2.5. 统计学处理
采用RevMan 5.3软件进行Meta分析。本研究结果数据均是连续型变量,采用均方差(MD)或标准化均方差(SMD)分析,均以95%CI表示。采用c2检验进行异质性分析,若P ≥ 0.1和I2 ≤ 50%,采用固定效应模型;若P < 0.1或I2 > 50%,采用随机效应模型或进行亚组分析,必要时进行敏感性分析,以判断结果的稳定性。若异质性过大且无法判断来源时,仅采用描述性分析。以P < 0.05为差异具有统计学意义。
3. 结果
3.1. 文献检索结果
初步检索获得517篇文献,再追溯参考文献1篇。最终纳入10篇文献进行Meta分析。见图1。
3.2. 纳入研究的基本特征及方法学质量评价
10项研究共纳入624例新生儿,其中母乳组309例,对照组315例。纳入研究的基本特征见表1,方法学质量评价见表2。
3.3. Meta分析结果
3.3.1. 操作性疼痛结局指标
1) 疼痛评分
4项研究 [10] [11] [14] [15] 以PIPP评分为结局指标,共229例新生儿。各研究间存在异质性(P = 0.03, I2 = 66%),采用随机效应模型,结果显示母乳组新生儿致痛性操作期间PIPP评分低于对照组,具有统计学差异[MD = −2.05, 95%CI = (−3.39, −0.72), P < 0.05],见图2。2项研究 [12] [13] 以NIPS评分为结局指标,共133例新生儿。各研究间不存在异质性(P = 0.32, I2 = 0%),采用固定效应模型,结果显示母乳组新生儿致痛性操作期间NIPS评分低于对照组,具有统计学差异[MD = −2.45, 95%CI = (−3.06, −1.84), P < 0.05],图略。
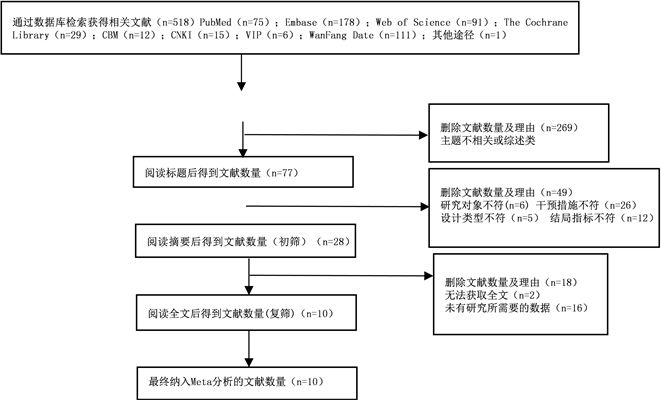
Figure 1. Document retrieval and screening process
图1. 文献检索及筛选流程

Table 1. Basic characteristics of included studies
表1. 纳入研究的基本特征
注:T:试验组;C:对照组;结局指标:A:心率;B:血氧饱和度;C:早产儿疼痛评分简表(Premature Infant Pain Pmfile, PIPP);D:新生儿疼痛评分量表(Neonatal Infant Pain Scale, NIPS);E:啼哭持续时间;F:出院时体重;G:达经口喂养过渡时间。

Table 2. Evaluation of methodological quality included in the study
表2. 纳入研究的方法学质量评价
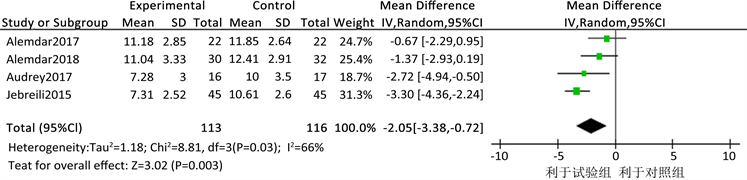
Figure 2. Effect of olfactory stimulation of human milk on PIPP score during neonatal painful operation
图2. 母乳嗅觉刺激对新生儿致痛性操作期间PIPP评分的影响
2) 血氧饱和度
4项研究 [4] [10] [12] [13] 评价母乳嗅觉刺激对新生儿致痛性操作期间血氧饱和度的影响,共237例新生儿。各研究间存在较大异质性(P = 0.0001, I2 = 88%),采用随机效应模型,为检验异质性来源,将母乳量分2 ml和5 ml进行亚组分析。2项研究 [4] [13] 结果显示2 ml母乳组新生儿致痛性操作期间血氧饱和度高于对照组,具有统计学差异[MD = 1.56, 95%CI = (0.63, 2.49), P < 0.05]。2项研究 [10] [12] 结果显示5 ml母乳组与对照组相比无统计学差异[MD = 1.06, 95%CI = (-0.94, 1.05), P > 0.05],见图3。

Figure 3. Effect of olfactory stimulation of human milk on blood oxygen saturation during neonatal painful operation
图3. 母乳嗅觉刺激对新生儿致痛性操作期间血氧饱和度的影响
3) 心率
4项研究 [4] [10] [12] [13] 评价母乳嗅觉刺激对新生儿致痛性操作期间心率的影响,共237例新生儿,由于合并结果异质性过大(P < 0.00001, I2 = 95%),不能判断异质性来源,因此仅采用描述性分析。1项 [12] 研究显示母乳组心率高于对照组,具有统计学差异;1项 [10] 研究显示母乳组与对照组心率无统计学差异;2项 [4] [13] 研究显示母乳组心率低于对照组,具有统计学差异,见图4。

Figure 4. Effect of olfactory stimulation of breast milk on heart rate during painful operation in neonates
图4. 母乳嗅觉刺激对新生儿致痛性操作期间心率的影响
4) 哭闹持续时间
3项研究 [10] [11] [13] 评价母乳嗅觉刺激对新生儿致痛性操作期间哭闹持续时间的影响,共161例新生儿。各研究间存在异质性(P < 0.0001, I2 = 98%),采用随机效应模型,结果显示两组新生儿致痛性操作期间哭闹持续时间无统计学差异[MD = −38.76, 95%CI = (−96.89, 19.37), P > 0.05],见图5。
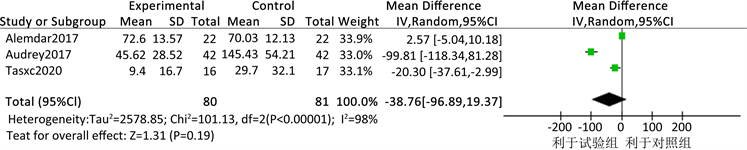
Figure 5. Effect of olfactory stimulation of breast milk on the duration of crying during painful operation in neonates
图5. 母乳嗅觉刺激对新生儿致痛性操作期间哭闹持续时间的影响
3.3.2. 喂养结局指标
1) 达经口喂养过渡时间
2项研究 [17] [18] 评价母乳嗅觉刺激对新生儿达经口喂养过渡时间的影响,共142例新生儿。各研究间不存在异质性(P = 0.55, I2 = 0%),采用固定效应模型,结果显示母乳组新生儿达经口喂养过渡时间短于对照组[MD = −2.28, 95%CI = (−3.89, −0.67), P < 0.05],具有统计学差异。
2) 出院时体重
2项研究 [17] [18] 评价母乳嗅觉刺激对新生儿出院时体重的影响,共142例新生儿。各研究间不存在异质性(P = 0.94, I2 = 0%),采用固定效应模型,结果显示两组新生儿出院时体重无统计学差异[MD = −2.28, 95%CI = (−65.81, 14.21), P > 0.05]。
3.4. 敏感性分析
由于以哭闹持续时间为结局指标的研究合并结果后存在较大的异质性,为检验合并结果的可靠性,采取逐一剔除某一项研究进行敏感性分析,评估新的合并效应量及异质性与剔除前结果有无显著差异。结果显示合并后异质性没有改变,说明结果比较可靠,见表3。

Table 3. Sensitivity analysis of olfactory stimulation of breast milk to crying duration during painful operation of newborn
表3. 母乳嗅觉刺激对新生儿致痛性操作期间哭闹持续时间的敏感性分析
4. 讨论
4.1. 母乳嗅觉刺激对新生儿操作性疼痛的影响
母乳含有糖类物质,能激活阿片类受体,释放5-羟色氨和多巴胺,缓解新生儿操作性疼痛,其气味刺激可舒缓新生儿的生理和心理状态 [19]。本研究结果显示,与新生儿常规护理相比,母乳嗅觉刺激可降低新生儿致痛性操作期间的疼痛评分,亚组分析结果显示2 ml的母乳量可提高新生儿致痛性操作期间的血氧饱和度,这可进一步证实母乳嗅觉刺激能稳定新生儿在应激状态下的生理指标,但5 ml母乳量对新生儿操作期间的血氧饱和度无影响,可能是由于新生儿的胎龄和干预方案差异引起。采用5 ml母乳量的两项研究 [10] [12] 的研究对象是早产儿和足月儿,且不是致痛性操作同一时间点上的结局指标,从而无法明确母乳对新生儿致痛性操作期间血氧饱和度的影响,有待进一步研究。新生儿具有嗅觉检测、辨别和记忆的能力,可以区分亲母和非亲母的母乳气味 [20] [21],基于新生儿高度敏感的嗅觉系统及母乳的天然特性,临床上将母乳气味作为一种个性化的非药物干预措施应用在新生儿护理中 [22] [23]。本研究中2 ml和5 ml的母乳量对新生儿致痛性操作期间血氧饱和度产生不一致的结论,可能是由于新生儿胎龄或干预方案差异引起。关于母乳干预的量,母乳距新生儿的距离及对新生儿致痛性操作期间心率和血氧饱和度的效果需要进一步验证。
4.2. 母乳嗅觉刺激对新生儿喂养的影响
本研究结果显示母乳嗅觉刺激可缩短新生儿达经口喂养过渡时间,促进喂养进程,但对新生儿出院时的体重无明显影响。母乳是胎儿出生后最佳的营养来源,其气味携带特异的挥发性化合物 [24],可快速诱导新生儿的觅食行为,引发吮吸–张口动作,使其尽早进行首次经口喂养 [6] [25]。另外,完全经口喂养取决于吸吮–吞咽–呼吸三者之间是否协调,重症监护室的新生儿受疾病和长期母婴分离的影响,自我调节能力弱,而母乳含有母亲的血液成分,携带着母亲的气味线索,当新生儿接触到母乳气味时,不仅有助于加强母婴联系,而且可稳定新生儿的生理和行为状态,提高喂养时的吸吮效率,促进吸吮–吞咽行为的发展,提高经口喂养的耐受性,进而缩短达经口喂养过渡和住院时间 [26] [27]。新生儿出院时的体重受胎龄、疾病等多种因素影响,由于本研究纳入的相关研究较少,母乳嗅觉刺激是否具有促进体重增加的优势,还需继续探索。
4.3. 研究局限性及对未来研究的启示
本研究局限性体现在:1) 纳入的高质量文献较少,由于母乳嗅觉刺激是行为干预,很难保证盲法的完全实施,存在偏倚的可能。2) 各研究干预方案在细节上存在差异,且结局指标测量的时点不一致。综上,母乳嗅觉刺激相比常规护理,可缓解新生儿操作性疼痛,促进喂养进程。但目前关于母乳嗅觉干预效果的高质量文献较少,建议未来采用更严谨的设计方案及干预流程,明确母乳干预的量、母乳距新生儿的距离、干预周期或频次、扩大临床应用范围,开展大样本、多中心的随机对照试验,进一步探究母乳嗅觉刺激对新生儿的临床应用效果。