摘要:
Naboth囊肿(Nabothian Cysts, NC)是子宫颈的良性病变,主要位于子宫颈的表面。巨大的NC罕见,而巨大的盆腔NC更罕见。我们报道了一例残角子宫切除术后的盆腔巨大Naboth囊肿,并复习相关文献,以加强妇科医生对盆腔NC存在的认识,并对该病的诊断及治疗提供参考。
Abstract:
Naboth cysts (Nabothian Cysts, NC) are benign lesions of the cervix, mainly located on the surface of the cervix. Huge NCs are rare, while huge pelvic NCs are even rarer. We reported a case of a giant Naboth cyst of the pelvic cavity after a residual angle hysterectomy, and reviewed the relevant literature, in order to strengthen the gynecologist’s understanding of the existence of pelvic NC, and provide references for the diagnosis and treatment of the disease.
1. 引言
Nabothian Cysts (NC)是子宫颈的良性病变。它是由宫颈柱状上皮细胞粘液分泌受阻而引起的潴留性囊肿。NC通常位于子宫颈表面,直径从几毫米到3~4厘米不等 [1]。囊肿的位置、大小以及与其他器官的关系决定其临床表现,进而影响其临床治疗的选择。本文,我们报告了一例残角子宫切除术后盆腔巨大NC,并复习既往中英文文献,均未见类似报道,本病例报道已获患者知情同意。
2. 临床资料
患者,39岁,因发现“盆腔肿物”2年,“宫颈原位腺鳞癌”2月入院。G5P2A3.既往月经规律。15年前因“残角子宫”行“残角子宫 + 右侧输卵管切除术”。患者2年前查体发现子宫右侧见约5.0 cm低回声团,考虑子宫肌瘤,患者无自觉不适,未予特殊处理。2月前复查,B超示:右附件区见5.8 × 5.7 × 4.2 cm低回声团,形态规则,边界清,CDFI:周边见点状血流信号,考虑阔韧带肌瘤可能(图1(A)、图1(B))。宫颈筛查,LCT:(−),HPV分型示:HPV16(+)。阴道镜下宫颈活检病理示:(宫颈12点)慢性子宫颈炎,部分区域复鳞上皮呈高级别上皮内病变(CINIII级)。LEEP (高频电波环切)术后病理示:(Leep环切宫颈)慢性灶状区域呈高级别鳞状上皮内病变(CINIII级),灶状区域呈产生粘液的复层上皮内病变(原位癌,具有腺、鳞双向分化)。肿瘤标记物未见明显异常,患者无腹痛、阴道异常流血、流液等不适,妇科查体示:宫颈轻度糜烂样改变,子宫右侧可扪及直径约6 cm大小包块,活动欠佳,轻压痛。
患者已完成生育,再无生育要求,且强烈要求切除子宫,遂行腹腔镜下筋膜外全子宫切除术 + 左侧输卵管切除术 + 盆腔肿物切除术。术中观察到,肠管广泛粘连于右腹壁、侧腹壁及后腹膜,在子宫颈右侧盆腔内见直径约6 cm大小囊性包块,表面光滑(图2(A),图2(B))。剖示该囊肿可见浓厚的巧克力样液体,清洗囊液后,囊壁光滑(图3(A),图3(B))。病理表明,在手术前被认为是宽韧带肌瘤的肿块被证实是NC。免疫组化Pax-8(−),P16(−),ER(+),PR(+),WT(−),Napsine(−)。(图4)患者术后半年复查未见明显异常。
3. 讨论
Nabothian囊肿(Nabothian Cysts, NC)是一种宫颈的良性病变 [1]。主要继发于宫颈慢性炎症的愈合过程,新生的鳞状上皮覆盖宫颈柱状上皮,导致柱状上皮分泌物引流受阻,形成潴留囊肿;当阴道内酸度和菌群改变时,Nabothian囊肿也有可能出现;接受孕激素治疗的患者可能由于宫颈粘液循环流动失败,而导致Nabothian囊肿的形成 [2] [3]。NC长到一定大小并通常会破裂,因此巨大的NC很少见。英文文献报道,直径大于4 CM的巨大NC仅8例,其中6例位于子宫颈和/或阴道,2例位于盆腔 [4] - [11]。
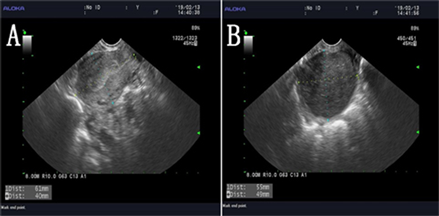
Figure 1. Ultrasound: A 5.8 × 5.7 × 4.2 cm hypoechoic mass in the right appendix area, with regular morphology and clear boundary
图1. 超声示:右附件区见5.8 × 5.7 × 4.2 cm低回声团,形态规则,边界清
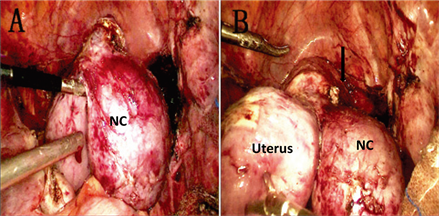
Figure 2. A 6 × 5 cm cystic mass on the right side of the cervix. ↓: Uterine vascular area
图2. 术中可见:子宫颈右侧6 × 5 cm的囊性肿块。↓:子宫血管区
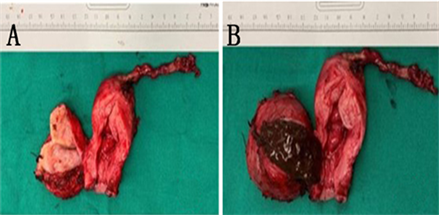
Figure 3. Thick chocolate-colored contents are seen in the sac; after removing the contents, the wall of the sac is smooth and the cavity is not connected to the uterine cavity
图3. 看到浓稠的巧克力色内容物;除去内含物后,囊壁是光滑的,并且腔未与子宫腔连接
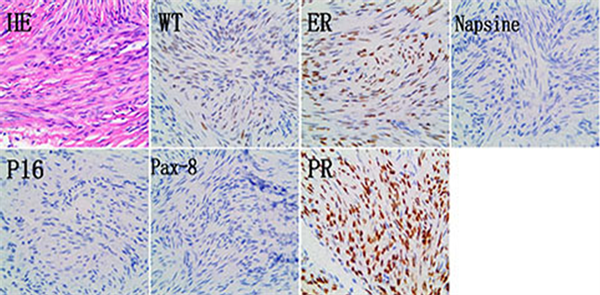
Figure 4. HE: The cyst wall is composed of a single layer of columnar cervical epithelial cells without obvious atypia. Napsine(−), ER(+), PR(+), Pax-8(−), WT(−). (400×)
图4. HE:囊壁由单层柱状宫颈上皮细胞组成,无明显异型性。Napsine(−),ER(+),PR(+),Pax-8(−),WT(−)。(400×)
本例患者Naboth囊肿直径约6 cm,位于子宫、宫颈右侧阔韧带内,囊肿根部位于子宫血管上方(图2(A)、图2(B)),临床上罕见。其具体形成原因不详。PhilipB.等对4例NC患者的分析发现NC可分布于宫颈的所有象限中,并占据宫颈管全长,同时可覆盖宫颈内壁全层直至宫颈浆膜层甚至可达宫颈旁的结缔组织,深部的囊肿,由于粘液潴留逐渐增大,对周围组织的压力增加,最终导致囊肿穿透的更深 [12]。也有文献指出筋膜内子宫切除术后若遗留少量宫颈管上皮,有可能形成直径约4~8 cm宫颈潴留囊肿 [13]。此患者15年前的手术记录表明,残留子宫的根部位于子宫体的右下侧,靠近该囊肿的根部。因此我们有理由怀疑,15年前的残角子宫切除术可能造成少量宫颈腺上皮异位到宫颈肌层或浆膜下,在长期慢性宫颈炎的修复过程中,导致宫颈柱状上皮分秘粘液排出受阻形成宫颈囊肿,后囊肿逐渐增大,并向右侧子宫阔韧带突出形成直径约6 cm的巨大囊肿。宫颈Naboth囊肿囊液常为粘稠清澈透明状,也可能由于合并感染而呈混浊脓性。本例囊肿术后剖视见囊内容物呈巧克力色粘稠胶冻样,临床上少见,使其易与子宫内膜残留引起的囊性子宫腺肌症相混淆 [14]。术前通过临床症状及影像学检查无法将两者鉴别,术中肉眼也无法将两者鉴别,最后唯有通过组织病理学明确诊断。文献指出多发的、大的Naboth囊肿可能与腺瘤的恶性分化有关 [7]。本例患者巨大Naboth囊肿与宫颈原位腺鳞癌并存,临床上少见。
典型的NC诊断相对容易,但是针对深部及盆腔NC的准确诊断则是困难的,但同时又是必要的。深部及盆腔NC可模仿附件及子宫肿瘤、宫颈恶性病变,准确的诊断可避免不必要的腹腔探查和子宫及附件切除 [15]。超声、CT、MRI均有助于深部及盆腔N.C的诊断 [3] [15] [16]。也有文献提出宫颈内超声较普通的超声更具有优势 [7]。值得一提的是MRI较其他影像学方法对深部及盆腔NC更敏感。其MRI表现为:T1W1低信号,T2W2高信号,囊壁光滑,无静脉强化,无实性结构 [16]。但是当借助现代诊断方法,不能完全排除恶性肿瘤时,可能依然需要腹腔探查和子宫切除 [7]。
4. 结论
盆腔巨大NC可以模拟子宫阔韧带肌瘤或附件肿瘤。由于位置特殊,难以依靠阴道镜和超声进行诊断,并且容易出现遗漏或误诊,建议进行MRI检查以提高其术前诊断的准确性。同时,妇科医生应加强对深部和盆腔NC存在的认识。简而言之,该病例报告是对盆腔NC存在的主要补充,也是对盆腔肿块性质鉴定的重要补充。